J Thorac Oncol:17年来,NSCLC病理报告的准确性和完整性随时间的变化
2021-07-21 MedSci原创 MedSci原创
通过合理设计的干预措施,可以有效识别、量化和提高NSCLC病理报告的质量
完整准确的病理报告对于手术的管理和预后预测均至关重要。本研究旨在评估不同类型医院的三种干预措施对手术切除后非小细胞肺癌 (NSCLC) 的病理报告的影响。
Trends in Accuracy and Comprehensiveness of Pathology Reports for Resected Non-small Cell Lung Cancer (NSCLC) in a High Mortality Area of the United States
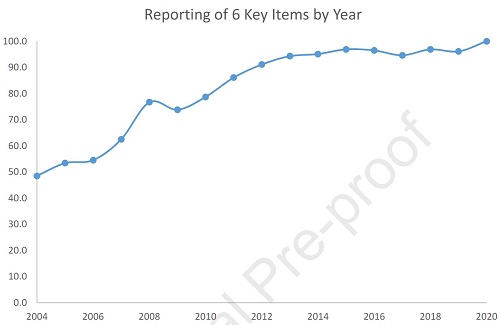
研究人员评估了2004年-2020年在美国4个州的11个医疗机构中接受NSCLC根治性手术切除的患者的病理报告在三种质量提高干预实施前后的完整性和准确性:教育(反馈提高意识)、天气报告和淋巴结标本采集试剂盒。研究人员在6个患者队列中对比了将病理报告的比例与术后管理最重要的六个项目(标本类型、肿瘤大小、组织学、病理 (p) T分类、pN分类、切缘状态)。
六项关键项目的完整性随时间的变化
在干预后时代,报告所有关键项目的完整性概率是干预前时代的8倍(OR 8.3; 95%CI 6.7-10.2;p<0.0001)。与干预前时代相比,干预后时代pT和pN分类的准确率分别增加了6倍和8倍(pT OR:5.7;pN OR:8.0;p<0.0001)。在干预组中,接受了三种干预措施的患者报告的所有六个关键项目、准确的pT分类和准确的pN分类的几率最高。
pT和pN分类的准确性随时间的变化
综上所述,该研究结果表明,通过合理设计的干预措施,可以有效识别、量化和提高NSCLC病理报告的质量。
原始出处:
Smeltzer Matthew P,Lee Yu-Sheng,Faris Nicholas R et al. Trends in Accuracy and Comprehensiveness of Pathology Reports for Resected Non-small Cell Lung Cancer (NSCLC) in a High Mortality Area of the United States.[J] .J Thorac Oncol, 2021, https://doi.org/10.1016/j.jtho.2021.06.027
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#完整性#
43
#准确性#
0
#THORAC#
33
#Oncol#
0
JTO上有很多不错的好文章,谢谢梅斯及时上新
52
谢谢梅斯分享这么多精彩信息
45
NSCLC下一步突破在于新靶点了,靶向治疗和免疫治疗基本见顶了,再有新的就需要新机制了
56