质子泵抑制剂(缩写为PPI)或称氢离子阻断剂,是一种抑制氢离子泵的药物,这种药物对于减少胃酸分泌的作用是显著且长效的,是现今减少胃酸分泌第二强效的药物,仅次于钾离子竞争性胃酸抑制剂(P-CAB)。
一直以来,PPI是许多胃肠道疾病的一线治疗,广泛用于治疗急、慢性消化系统酸相关性疾病,包括胃食管反流病(GERD)、卓-艾综合征、消化性溃疡、上消化道出血及相关疾病。自上世纪80年代起,质子泵抑制剂的发现已成为美国第三大处方药。
PPIs是目前公认的治疗酸相关性疾病最有效的药物;PPIs也是老年人的常用药物之一,近年来PPIs过度使用的问题日益突出,药物的不良反应受到密切关注。近几年来,已有不少研究显示,PPI的治疗会导致肠道菌群紊乱。
此外,2019年发表在胃肠病学顶尖杂志GUT上的研究表明,长期服用PPI会增加罹患胃癌的风险。但这项在中国香港展开的研究提示,长期使用PPIs仅与每年每1万人中的4例额外胃癌病例有关。
鉴于PPI的使用与根除幽门螺旋杆菌相关的胃癌之间的关联尚未在胃癌高风险的地理区域得到充分调查。近日,来自韩国翰林大学的研究人员开展了相关研究,旨在评估韩国的PPI和胃癌之间的关系。结果再次发表于GUT。
本研究分析了2002年至2013年韩国国家健康保险服务数据库的原始和通用数据模型版本。通过Cox比例危害模型比较了PPIs新用户和PPIs以外的其他药物的1年药物暴露后的胃癌发病率。同时还分析了PPI使用者在根除幽门螺杆菌后的胃癌发病率。
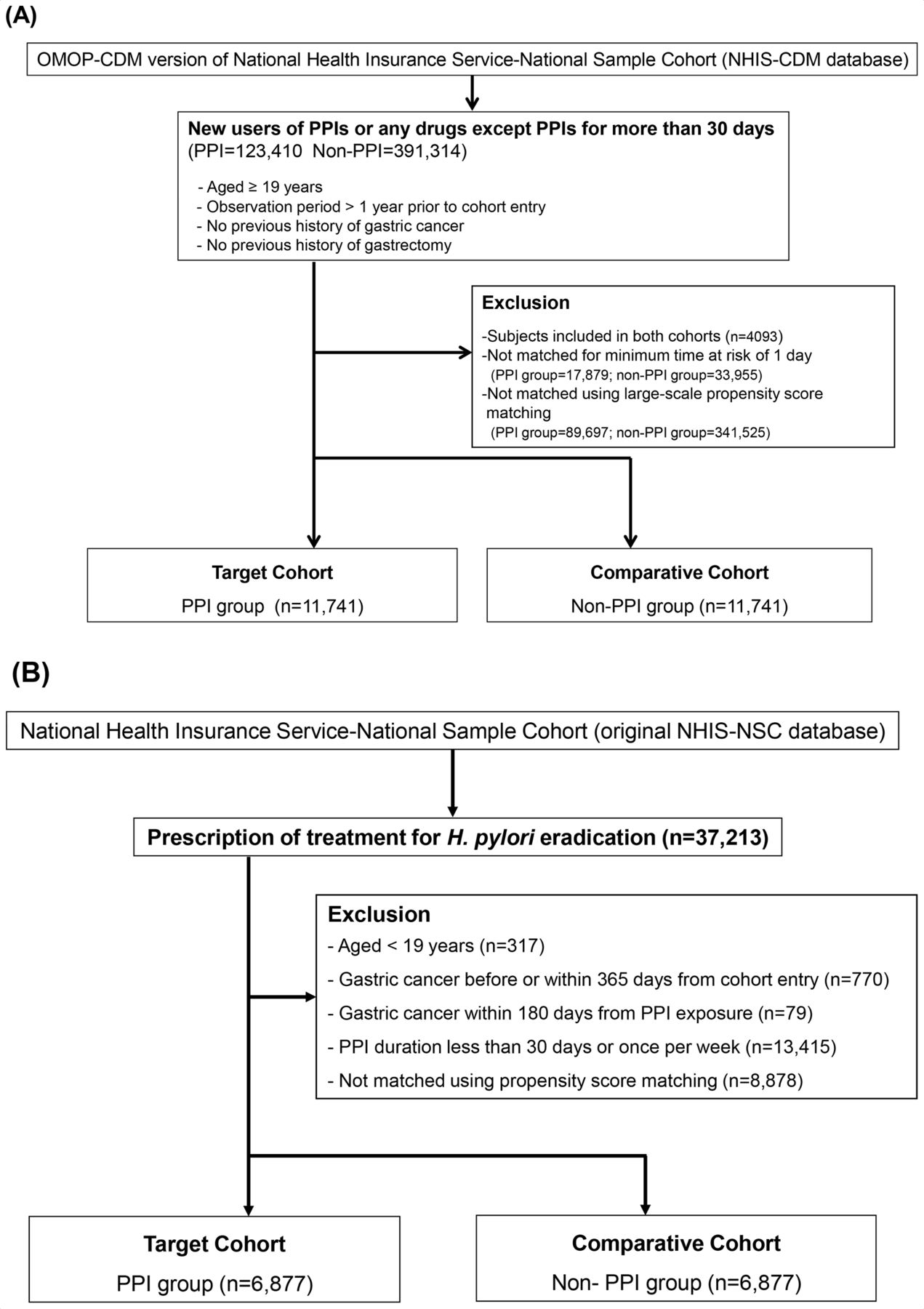
这是一项这是一项基于NHIS-NSC队列的回顾性研究。研究人员根据参与者的用药情况将其分为三组:1)暴露组——PPI组(连续使用PPI≥30天);2)非PPI组(连续使用不含PPI的药物≥30天);3)H2RA组(连续使用H2RA≥30天)。
最终包纳入括经过大规模倾向得分匹配后的PPI和非PPI队列的11741名患者。在4.3年的中位随访期间,使用PPI与胃癌发病率增加2.37倍有关(PPI≥30天vs非PPI;118/51813人年vs40/49729人年)。

同时胃癌的发病率与使用PPI的时间呈平行上升趋势,即使用时间越久,癌症风险越高。≥90天时,风险是非PPI组的2.83倍;≥365天时,风险是非PPI组的3.50倍。
在根除幽门螺杆菌的受试者中,与非PPI组相比,PPI使用超过180天可使胃癌的发病率升高120%(PPI≥180天vs非PPI;30/12470人年vs9/7814人年;HR=2.22)。
综上,该研究表明,不论是否根除幽门螺杆菌,长期使用PPI与胃癌风险升高有关。
参考文献:
Association between proton pump inhibitor use and gastric cancer: a population-based cohort study using two different types of nationwide databases in Korea. http://dx.doi.org/10.1136/gutjnl-2020-323845
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言



















#质子泵#
62
#抑制剂#
45
#癌风险#
33
学习了
54
#长期使用#
27
学到啦
69