低碳水化合物饮食,又称低糖饮食,是限制碳水化合物(糖类)摄入量的饮食方案,通常用于治疗肥胖或糖尿病。此饮食会限制精致碳水化合物的摄取(例如糖、面包、面食),改为食用蛋白质和脂类百分比高的食品(例如肉类、禽类、贝类、蛋类、奶酪、坚果、植物籽实类或花生)以及其他低碳水化合物的食品(如大多数拌沙律的蔬菜)。低碳水化合物饮食也允许食用其他类蔬菜和水果(特别是浆果类)。不同的低碳水化合物饮食方案允许食用的碳水化合物的量不同。
这种饮食有时是生酮饮食(限制碳水化合物的摄入量直到身体出现酮症),如阿特金斯健康饮食法的诱导阶段即为生酮饮食。不过,一些文献把某些限制变量较少的饮食方案也看作为“低碳水化合物”饮食方案。
除了治疗肥胖症以外,低碳水化合物饮食也用于治疗其他疾病,特别值得提出的是改善糖尿病和癫痫病但也用于治疗慢性疲劳综合症和多囊卵巢综合症以及癌症。
近期,为了确定低碳水化合物饮食(LCD)和极低碳水化合物饮食(VLCD)对2型糖尿病(T2DM)患者的疗效和安全性,来自美国德克萨斯A&M大学营养学专家展开了系统回顾和荟萃分析,结果发表在《英国医学杂志》BMJ上。
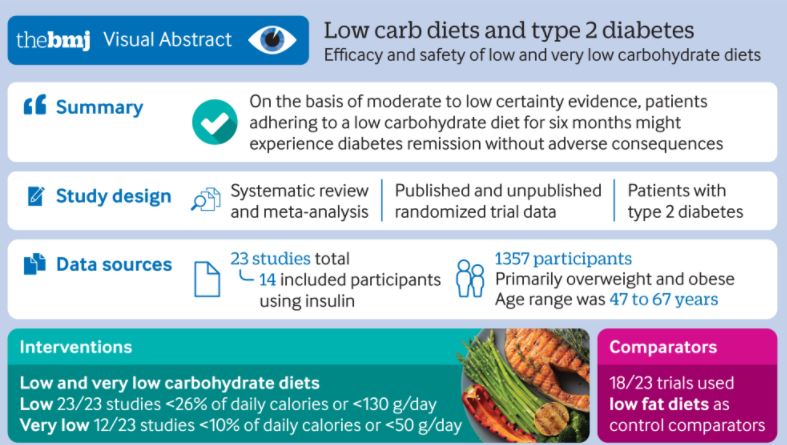
研究人员搜索CENTRAL、Medline、Embase、CINAHL、CAB等数据库文献来源,主要选择对T2DM患者的LCD(<130克/天或<26%的2000千卡/天的饮食)和VLCD(<10%的碳水化合物热量)进行评估至少12周的随机临床试验。
主要的实验设计图
主要结果是糖尿病的缓解(HbA1c<6.5%或空腹血糖<7.0mmol/L)、体重减轻、HbA1c、空腹血糖和不良事件。次要结果包括与健康有关的生活质量和生化指标。
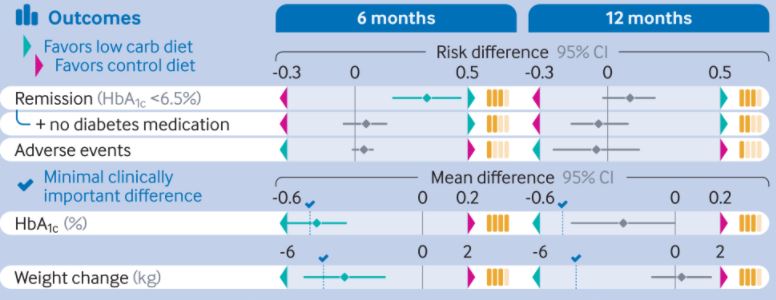
共搜索确定了14759篇文献,纳入23项试验(1357名参与者),40.6%的结果被判定为低偏倚风险。在6个月时,与对照组饮食相比,LCD取得了更高的糖尿病缓解率(HbA1c<6.5%)(76/133(57%)vs 41/131(31%);风险差异0.32)。
6个月和12个月LCD和VLCD饮食HbA1c和体重变化的差异
6个月时,体重减轻、甘油三酯和胰岛素敏感性都有较大临床意义的改善,但在12个月时差异减少。同时,VLCD在6个月时对体重减轻的效果不如限制性较低的LCD。然而,这种影响是由饮食的依从性解释的。也就是说,高度坚持VLCD的患者较不太坚持的人体重有了临床意义的减少。
由此可见,坚持6个月低碳水饮食的患者糖尿病的缓解率较高,而不会产生不良后果。
参考文献:
Efficacy and safety of low and very low carbohydrate diets for type 2 diabetes remission: systematic review and meta-analysis of published and unpublished randomized trial data. BMJ 2021; 372 doi: https://doi.org/10.1136/bmj.m4743
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#BMJ#
0
好
57
好
52
挺好
55
谢谢MedSci提供最新的资讯
43
zsbd
61
学习
37