CARDIOVASC DIABETOL:糖化白蛋白(GA)对NSTE-ACS患者经皮冠状动脉介入治疗的预后意义
2022-02-03 MedSci原创 MedSci原创
近年来,糖化白蛋白(GA)由于不受食物摄入和红细胞寿命的影响而受到广泛关注,GA一般反映2-4周的血糖控制状况。
近年来,糖化白蛋白(GA)由于不受食物摄入和红细胞寿命的影响而受到广泛关注,GA一般反映2-4周的血糖控制状况。然而,GA对非ST段抬高急性冠状动脉综合征(NSTE-ACS) 患者进行经皮冠状动脉介入治疗(PCI)中的预后价值存在很大程度的不确定性。此外,缺乏比较FBG、HbA1c和GA对心血管不良预后的预测价值的研究。因此,本研究旨在评估GA对NSTE-ACS患者PCI术后不良预后的预测价值。

本研究最终纳入了首都医科大学北京安贞医院2015年1月至12月接受PCI的2247例 NSTE-ACS 患者。对所有患者进行随访直至患者换死亡或出院后48个月。主要结局是不良心脑事件(MACCEs),包括全因死亡、非致死性心肌梗死、缺血诱导的血运重建和非致死性缺血性卒中。
随访期间共记录了547例(24.3%)MACCE。结果显示,GA水平高的个体与GA水平低的个体相比,MACCEs的发病率显著升高。在校正混杂因素后,GA增加仍然是研究人群中不良预后的重要独立预测因子。将遗传算法添加到包含传统危险因素的模型中,显著提高了预测预后不良风险的能力。
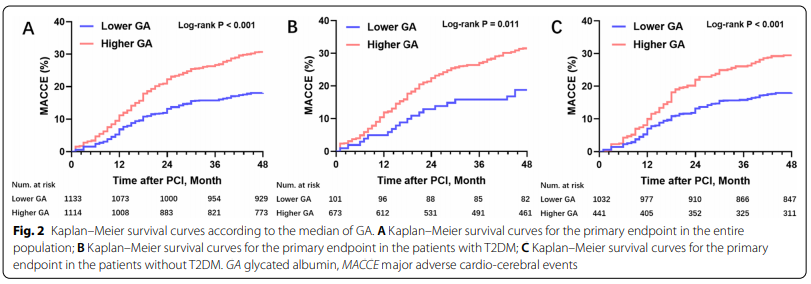
根据GA的中位数得到Kaplan-Meier生存曲线
总而言之,本研究证实,在接受PCI治疗的NSTE-ACS患者中,GA水平与不良心脑事件的高风险显著相关。GA的加入显著提高了传统风险模型预测不良预后的能力。这一结论需要进一步的前瞻性、大规模的研究来证实。
参考文献:Liu, C., Zhao, Q., Ma, X. et al. Prognostic implication of serum glycated albumin for patients with non-ST-segment elevation acute coronary syndrome undergoing percutaneous coronary intervention. Cardiovasc Diabetol 21, 11 (2022). https://doi.org/10.1186/s12933-022-01446-3
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#ASC#
37
#BET#
37
#DIA#
43
#NSTE-ACS#
42
#冠状动脉介入治疗#
49
#NST#
37
#ACS#
37
#白蛋白#
44
#经皮冠状动脉介入治疗#
33
#预后意义#
43