NEJM:TAVR后念珠菌性心内膜炎-病例报道
2019-01-03 xing.T MedSci原创
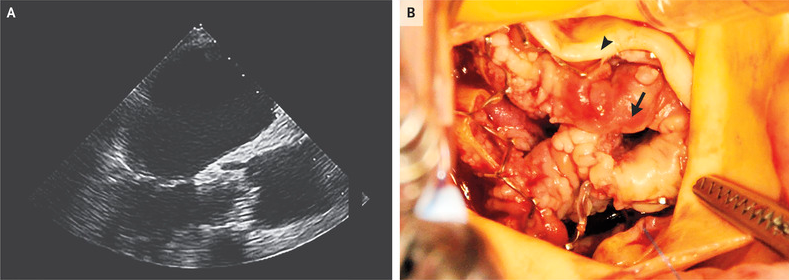
经食道超声心动图(如图A所示)证实为人工瓣膜心内膜炎,其显示大量赘生物导致人工瓣膜严重受阻(跨瓣平均压力梯度为52 mmHg;主动脉瓣面积为0.5cm2)。
患者为一名有充血性心力衰竭病史且射血分数为45%的76岁男性,因呼吸急促而到急诊就诊。他在9个月前接受了经导管主动脉瓣置换术(TAVR)。
他的体温为39.0°C,在心脏检查中检测到5级收缩期杂音(伴有可触知的震颤)。胸部X线片显示与肺水肿一致的变化。实验室检查结果值得注意的是白细胞计数为每立方毫米16,000个细胞(参考范围为4000到10000),C反应蛋白水平为120毫克/升(参考范围<5)。
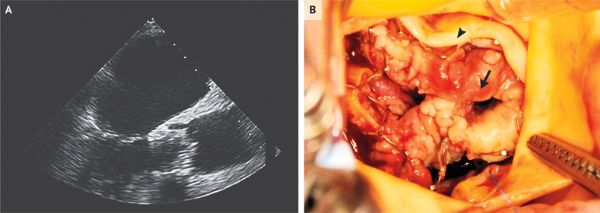
该患者进行外科主动脉瓣置换,观察到赘生物(如图B箭标所示)和原生小叶(如图B箭头所示)。手术部位的伤口感染使术后病程复杂化。患者出院但4周后因肺炎再次入院。在住院2个月后,他死于呼吸系统疾病。
原始出处:
Thierry Carrel, et al.Candida Endocarditis after TAVR.N Engl J Med 2018;https://www.nejm.org/doi/full/10.1056/NEJMicm1809948
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#念珠菌#
29
#内膜#
35
#AVR#
35
#心内膜炎#
32
谢谢分享,学习了
69