第五届呼吸危重症论坛:范红:中国成人医院获得性肺炎与呼吸机相关性肺炎(HAP/VAP)诊断和治疗指南(2018)解读
2019-03-25 Fiona MedSci原创
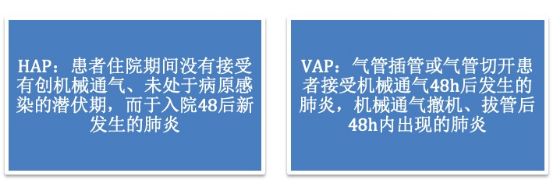
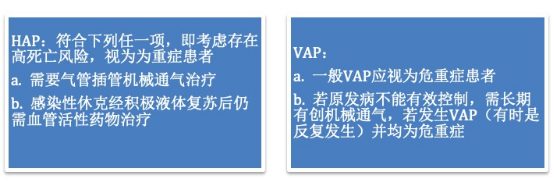
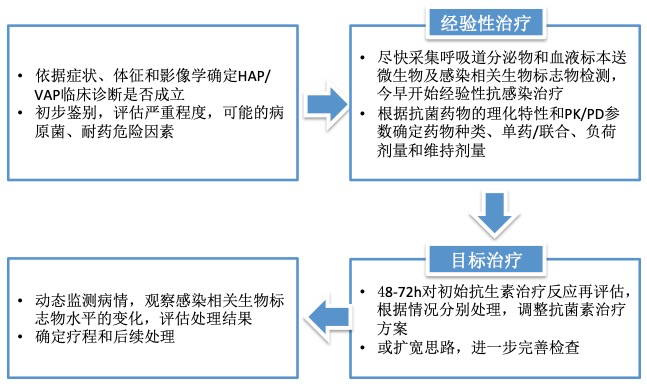
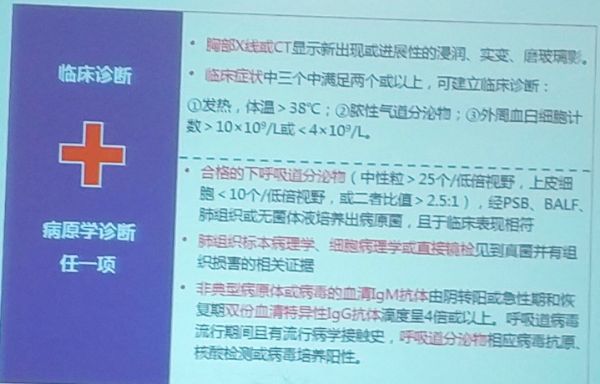
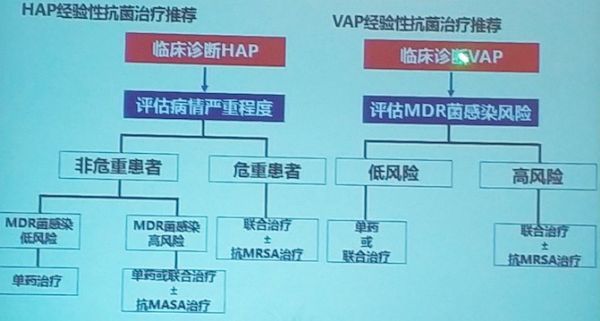
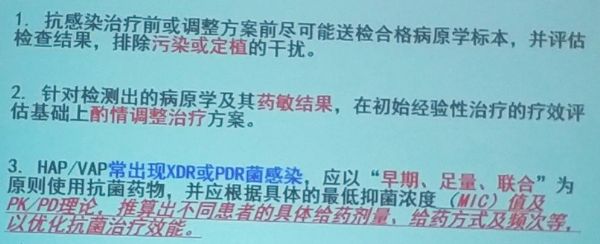
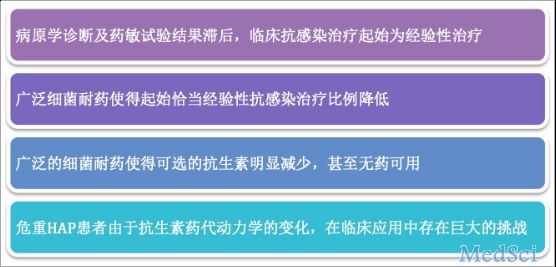
在CTS指南的HAP及VAP概念中不再区分早发和晚发:?医疗机构相关性肺炎(HCAP)不作为HAP的一个独立类型。?呼吸机相关性支气管炎(VAT):接受有创机械通气48小时后出现的细菌性气管支气管炎。不建议将VAT作为特定类型的临床诊断而启动抗菌药物治疗我国HAP/VAP的流行病学中,HAP/VAP在内的下呼吸道感染居医院获得性感染构成比之首。国内外研究均表明:多重耐药MDR或全耐药PDR菌的归隐


本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









受益匪浅
45
#治疗指南#
27
#VAP#
34
#获得性#
20
#相关性#
34
呼吸危重症论坛。
58
呼吸危重论坛。
54
#呼吸机#
27