病例分享:1例ALK重排肺鳞癌患者的治疗
2018-07-15 江美林 蒲兴祥(湖南省肿瘤医院/中南大学湘雅医学院附属肿瘤医院) 中国医学论坛报今日肿瘤
患者男性,46岁,2016年3月31日因“咳嗽、咳痰1月”初诊我院。既往吸烟史20年,余无特殊。
病例简介
患者男性,46岁,2016年3月31日因“咳嗽、咳痰1月”初诊我院。既往吸烟史20年,余无特殊。
体格检查
ECOG评分1分。一般情况可,颈面部皮肤潮红、肿胀,颈静脉充盈,胸壁浅表静脉曲张;双锁骨上、双颈部未及肿大淋巴结。余无特殊。
诊治经过
入院查血常规、肝肾功能、电解质、血糖、凝血功能基本正常。
肿瘤标志物:糖类抗原(CA)125、CA153升高。
胸部CT:右上肺前段结节影;双侧锁骨上区、纵隔内及双肺门多发肿大淋巴结,考虑转移;双侧胸腔积液,心包积液,考虑转移(图1)。
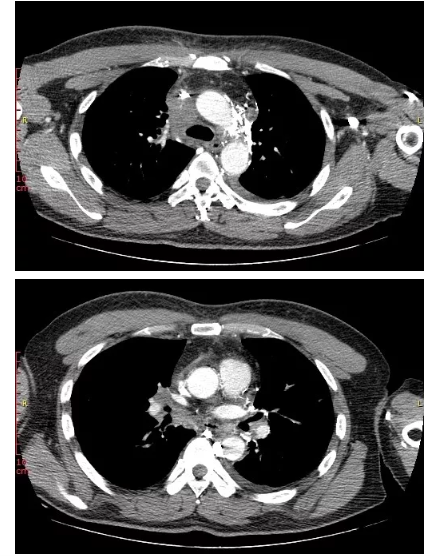
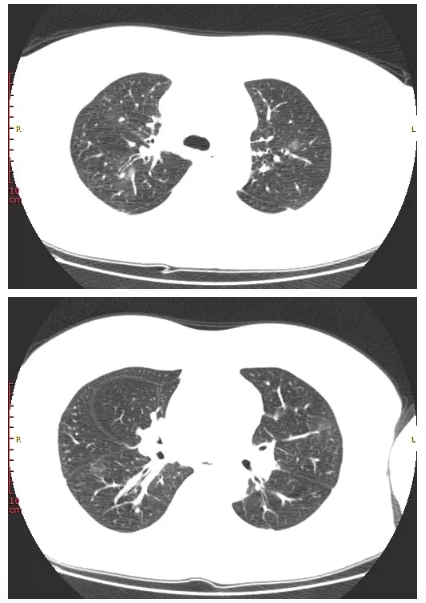
图1 胸部CT(2016年3月31日基线)
脑磁共振成像(MRI):右侧脑室后角后下方强化结节,考虑转移瘤(图2)。
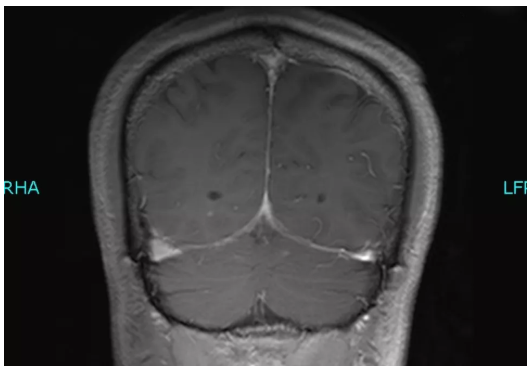
图2 脑MRI(2016年4月6日基线)
骨显像:胸骨体局部、左侧第9后肋放射性异常增浓,考虑转移瘤。
EBUS-TBNA病理检查:4R及隆突下淋巴结穿刺物结果支持低分化鳞癌。
诊断:右上肺中央型鳞癌,T4N3M1,Ⅳ期,伴有双侧锁骨上区、纵隔内、双肺门多发淋巴结转移、胸膜转移、心包转移、脑转移、骨转移。
入院后2016年4月3日开始行TP方案(紫杉醇脂质体295 mg、d1,顺铂46 mg、d1~3,恩度30 mg、d1~7)化疗2周期;同时2016年4月14日~4月28日予胸部姑息放疗(剂量:95% PTV 30 Gy/10 f),肺部病灶、纵隔及双颈部多发肿大淋巴结同前,双侧胸腔积液较前稍增多,疗效评价为疾病稳定(SD)(图3)。
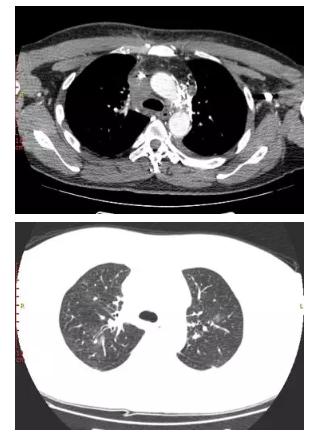
图3 化疗2周期后复查胸部CT
基因检测(NGS)结果提示为EML4-ALK复杂重排,补做免疫组化示ALK(+),于2016年5月27日开始口服克唑替尼靶向药物,服用2个月时复查发现肺部病灶稳定,胸水增多,左侧脑部有新发病灶,疗效评价为疾病进展(PD)(图4)。
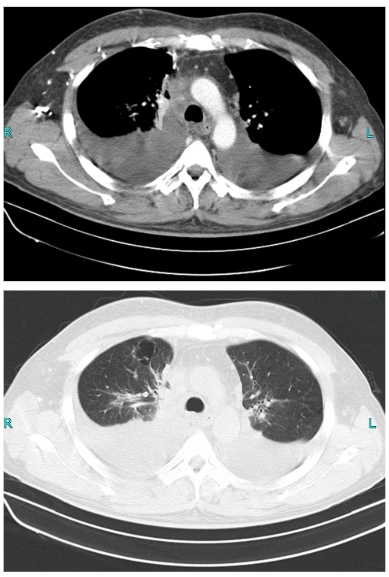
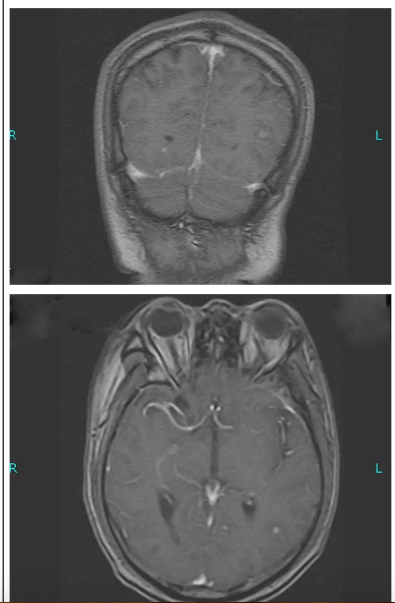
图4 克唑替尼治疗2个月后复查胸部CT和脑部MRI
后患者自行购买并于2016年8月1日开始服用第二代ALK抑制剂brigatinib(具体剂量不详),期间规律复查,病灶持续稳定,最佳疗效评价为SD,但治疗6个月时复查发现肺部病灶较前增大,脑部转移灶消失,提示病情进展(图5)。
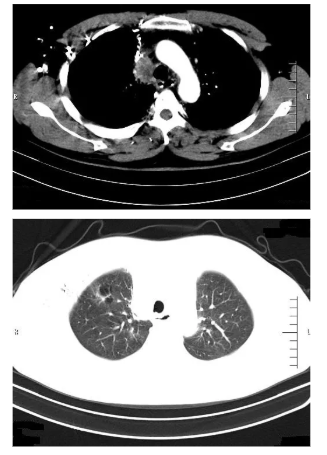
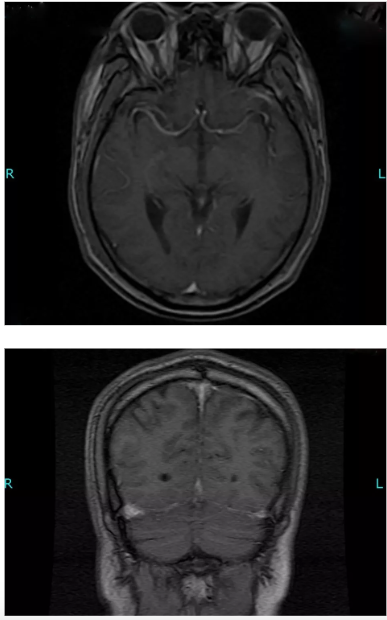
图5 Brigatinib治疗6个月时复查胸部CT和脑部MRI
患者第二次基因检测(血液)结果只有RB1基因突变,后于2017年3月24日开始行GP方案(吉西他滨2.2 g,d1、d8;顺铂130 mg,d1)化疗2周期,肺部原发灶较前增大,脑新增多发转移灶,疗效评价为PD。后患者进行了第三次基因检测(血液),结果与第二次一样。患者于2017年5月11日开始自行brigatinib加量治疗(具体剂量不详),服用4个月后病情再次进展(图6)。
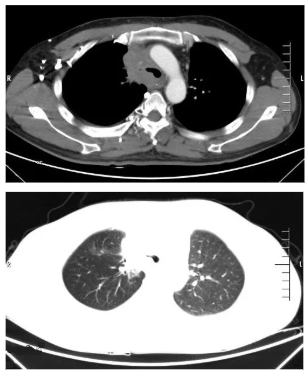
图6 Brigatinib加量治疗4个月时复查胸部CT
后患者自行购买并服用劳拉替尼原料药1个月后又再次进展,患者第四次胸水和血液基因检测结果都显示EML4-ALK融合。后患者选择行培美曲塞单药(800 mg、d1)化疗1周期,最终患者因肺部感染于2018年2月9日去世。
病例小结
这是一例特殊的肺鳞癌患者靶向治疗病例,中年男性,患者入院诊断为肺鳞癌Ⅳ期EML4-ALK复杂融合;初诊时一般情况较好,ECOG评分1分;经济情况好。
患者入院后一线予紫杉醇+顺铂+恩度化疗2周期和胸部姑息放疗,评效为SD;后患者基因检测及免疫组化结果提示ALK融合,遂要求行克唑替尼靶向治疗,但服用2个月后疾病进展;之后患者4次发生疾病进展,分别是brigatinib治疗6个月时、吉西他滨+顺铂化疗2周期后、brigatinib加量治疗4个月时和劳拉替尼原料药治疗1个月时。同时患者分别在不同疾病进展时期进行了4次基因检测,没有获得具有太多治疗指导价值的结果,最终经过多线综合治疗后因肺部感染去世。
治疗体会
众所周知,EML4-ALK重排在非小细胞肺癌基因突变中所占比例较少,而肺鳞癌中发生率更低,约为0~2.5%。临床病理学分析显示,在非小细胞肺癌中,ALK重排多发生于吸烟史无或短、确诊年龄小、无EGFR突变的腺癌等患者。本病例是一位有ALK重排并有长期吸烟史的中年肺鳞癌患者,基线组织标本基因检测结果显示EML4-ALK-FAM168B复杂重排。这三个基因复杂重排是在ALK断点所在位置(19号内含子),与肺癌中经典的EML4-ALK融合基因内常见发生断裂的位置相一致,但从基因重排方向上来看,在ALK断点处,同时与另一个基因FAM168B发生重排,三个基因间有较为复杂的重排关系。患者经过两个周期一线同步放化疗后疗效评价为SD,克唑替尼、brigatinib和劳拉替尼原料药的治疗效果也在相关临床试验生存数据的预期之下,出现这种情况可能有很多因素的影响,包括EML4-ALK复杂重排形式、未检测的新的耐药性突变。然而,除了进一步的精确检测,关于这种重排形式的更多细节我们无从知晓。总而言之,需要更多的生物医学与临床方面的研究来阐明这种少见ALK重排形式对肺鳞癌患者治疗的意义。
从该肺鳞癌患者的ALK抑制剂靶向治疗过程中,可以发现二代ALK抑制剂治疗脑转移灶的疗效确实优于一代ALK抑制剂。患者服用克唑替尼2个月后因脑部新发转移瘤而进展,肺部原发灶仍然稳定;但无论是经过brigatinib治疗还是劳拉替尼原料药治疗,患者都因肺部原发灶增大而进展,脑部转移灶消失。故证实了二代ALK抑制剂对于克唑替尼耐药和脑转移的ALK阳性肺癌患者有显著疗效,为其他类似患者提供治疗指导价值。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#鳞癌患者#
37
#肺鳞癌#
36
#鳞癌#
46
了解一下.谢谢分享!
69
学习了.谢谢分享.
79