Nat Commun:靶向Gα13介导的整合素信号可有效改善全身性炎症
2021-05-28 xiaozeng MedSci原创
细菌感染(如败血症)或病毒感染均可引发全身性炎症反应综合征。在该状态下,白细胞和巨噬细胞会释放出大量的细胞因子(细胞因子风暴)、氧化剂和其他促炎因子,这些因子不仅会引起全身性炎症反应和血管渗漏/出血,
细菌感染(如败血症)或病毒感染均可引发全身性炎症反应综合征。在该状态下,白细胞和巨噬细胞会释放出大量的细胞因子(细胞因子风暴)、氧化剂和其他促炎因子,这些因子不仅会引起全身性炎症反应和血管渗漏/出血,且还会引起血栓形成。
炎症反应、血管渗漏和血栓形成会共同导致多器官功能障碍,包括急性呼吸窘迫综合征(ARDS)、肾衰竭、弥散性血管内凝血(DIC)和循环系统衰竭。
根据疾病控制中心(Centers for Disease Control)的数据显示,死于医院的患者中有三分之一患有败血症,在美国,每年至少有170万成年人患败血症,且约270,000例病例中该病是致命的。
因此,迫切需要用于治疗全身性炎症的新型药物。尽管目前已进行了一系列深入的研究和大量的临床试验,但仍未发现有效的治疗全身性炎症的药物。
基于相关的基础和临床研究,研究人员假设炎症、血管渗漏/出血和血栓形成除了相互依存加剧外,还会独立的导致系统性炎症的不良预后。该假设还表明,在治疗全身性血栓性炎症的情况下,在不加重血管渗漏/出血的情况下,能够更有效地靶向炎症和血栓形成。
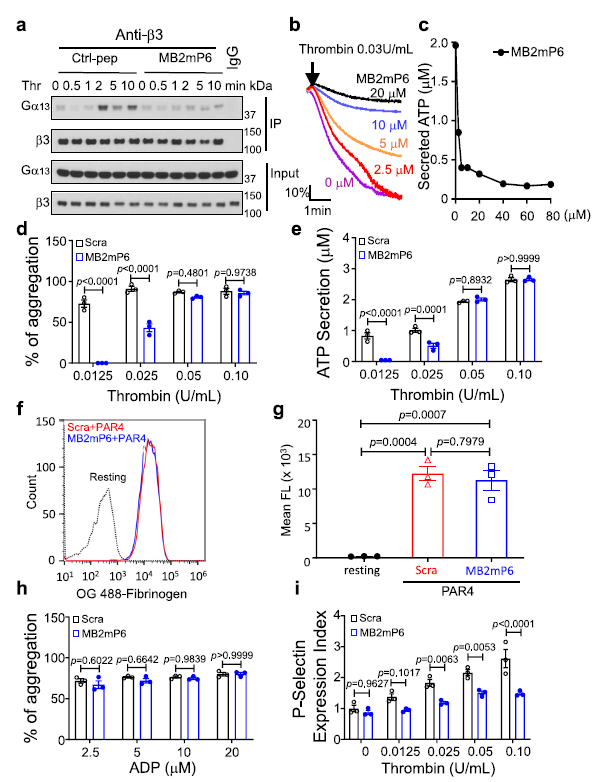
MB2mP6抑制Gα13与β3整合素相互作用及血小板的功能
在该研究中,研究人员发现,在白细胞和血小板中,靶向Gα13介导的整合素信号的MB2mP6纳米颗粒的使用,既能够抑制炎症和血栓形成,又不会引起血管渗漏/出血。
在严重脓毒症发作的小鼠模型中,立即或数小时后灌输MB2mP6可改善小鼠的存活率。此外,血小板中敲除Gα13可抑制败血性血栓的形成,而白细胞中敲除Gα13则可减少败血性炎症的发生,二者均可适度的提高生存率。而血小板和白细胞双敲除Gα13能够抑制败血性血栓的形成和炎症的发生,并进一步提高生存率,表现出与MB2mP6类似的效果。
MB2mP6可抑制肺血管渗漏
总而言之,该研究结果表明,炎症和血栓形成事件能够独立的导致不良预后并加重全身性炎症,该研究还揭示了双重抗炎/抗血栓形成疗法的概念,该疗法并不会加剧血管渗漏的发生。
原始出处:
Cheng, N., Zhang, Y., Delaney, M.K. et al. Targeting Gα13-integrin interaction ameliorates systemic inflammation. Nat Commun 12, 3185 (27 May 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Nat#
32
#COMMUN#
34
#整合素#
42
真棒
45