Front Oncol:III期临床研究XELAVIRI评估一线贝伐珠单抗为基础的续观治疗对比联合治疗转移性结直肠癌(mCRC)患者的疗效
2022-02-23 yd2015 MedSci原创
研究表明,初始贝伐珠单抗联合治疗可改善转移性结直肠癌(mCRC)患者的ETS 和DpR。ETS可作为其预后指标。
近期,德国团队在Frontiers in Oncology杂志上发表了一项研究成果,主要是回顾性分析III期临床研究XELAVIRI的数据,评估转移性结直肠癌(mCRC)患者一线使用贝伐珠单抗为基础的续观治疗或联合治疗的疗效。
研究分析DpR(从基线到最小肿瘤直径的变化)、ETS(首次重新评估时肿瘤直径减少≧20%)和治疗至DpR的时间(研究随机化开始到DpR的时间)。我们根据治疗组、分子亚群,性别和ETS作为分层参数评估无进展生存期和总生存期。
在改良意向治疗组(mITT)的421名患者中,有370名患者,其中序贯治疗组为186/212(87.7%)患者,初始联合治疗组为184/209(88.0%)患者可用DpR和ETS评估。在这370名患者中,有330人可以获得分子亚型(RAS和BRAF状态)的信息。
与初始续观治疗组相比较,初始联合治疗在第一次影像学评估时获得显著更高的DpR (-40.0% vs -24.7%;p <0.001)和更高中位ETS发生率[60.9% vs. 43.5%;OR=2.00,95%CI:1.33-3.03,P = 0.001]。使用BRAF MT、RAS MT、年龄和性别作为协变量进行多变量分析时,这些差异仍具有统计学意义 [DpR: p < 0.001; ETS: OR 5.68 (95% CI: 3.57–13.16); p = 0.001]。
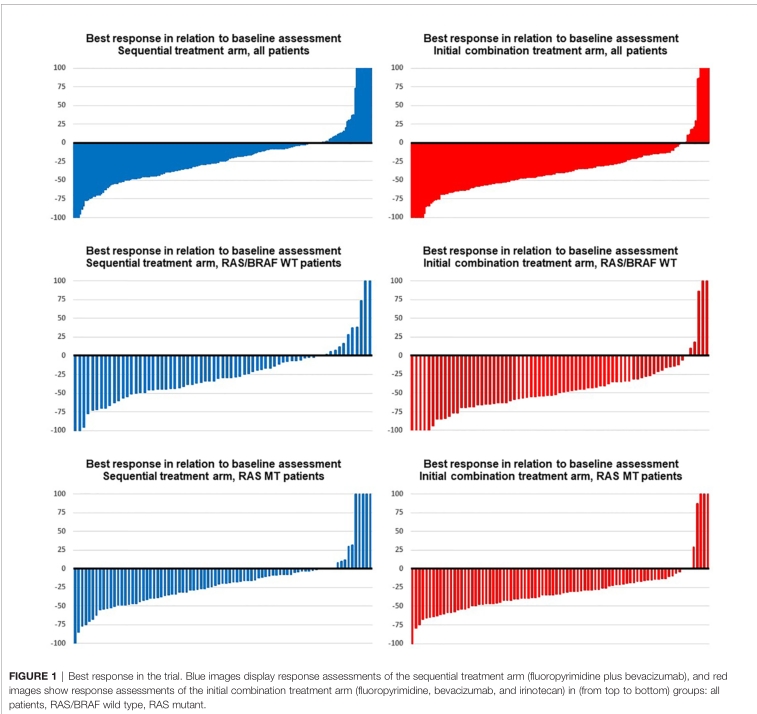
在突变状态方面,RAS野生型(RAS WT)和BRAF野生型(BRAF WT) mCRC患者接受联合治疗的中位DpR显著增加(-49.6% vs -29.3%;p<0.001), ETS频率更高[72.6% vs. 50.7%;OR=2.56,95%CI:1.28 5.26;P = 0.002]。治疗组仍然是 RAS/BRAF WT患者DpR (p = 0.009)和ETS[OR 5.53 (95% CI: 2.99 34.48);p = 0.020]改善的独立因素。
男性患者与女性mCRC患者相比,在初始联合治疗中,中位DpR显著受益(男性:-40.0% vs -22.2%;p<0.001;女性:-34.0% vs. -24.4%;p = 0.13)和ETS发生率[男性:64.8% vs. 40.2%;OR=2.78,95%CI:1.64 4.55);p<0.001;女性:52.5% vs 49.3%;p = 0.73)。在多变量分析中,这些差异仍具有统计学意义[DpR: p < 0.001; ETS: OR=4.24 (95% CI: 2.78–8.93); p < 0.001]。
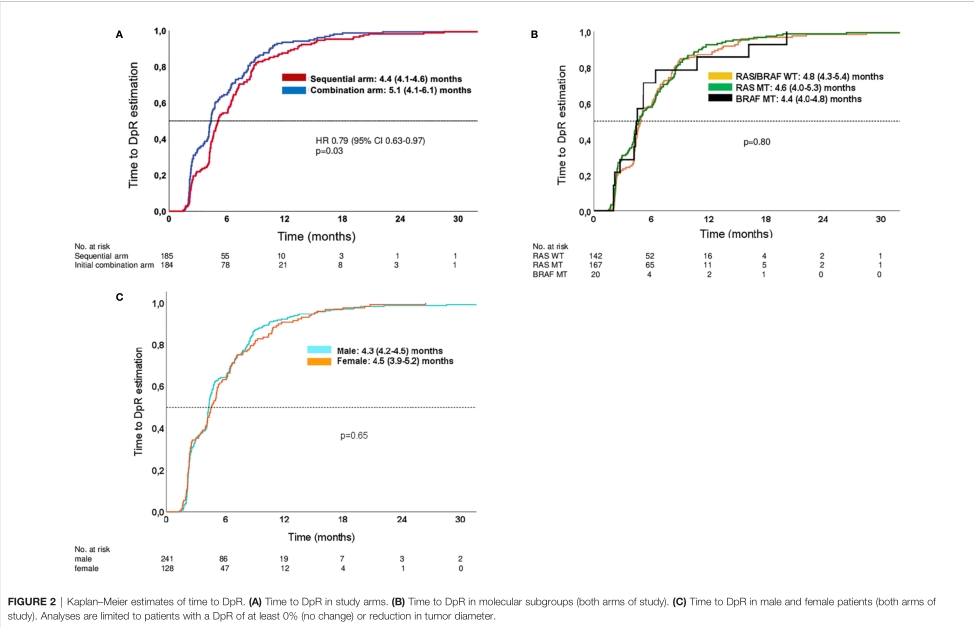
与初始联合治疗组相比,序贯治疗组患者的DpR时间显著缩短[4.4个月(95% CI: 4.1 4.6个月) vs 5.1个月(95% CI: 4.1 6.1个月);p = 0.03)。
ETS与PFS改善[无ETS: 8.2个月(7.6-8.8个月);ETS: 11.9个月(10.2-13.5个月);log-rank p<0.001]和OS改善[无ETS: 21.2(18.8-23.6)个月;ETS: 28.5个月(25.2-31.8个月);Log-rank p = 0.002]相关。当调整治疗组、性别、年龄、RAS突变和BRAF突变时,这些生存差异仍具有统计学意义[PFS: p<0.001;HR 0.618 (95%CI 0.499-0.767);OS: p = 0.003;HR 0.713 95%CI 0.568-0.895)]。
ETS与延长的生存时间相关,而无论治疗方式(PFS: log-rank p<0.001;OS: log-rank p=0.012)和分子亚组(PFS: log-rank p<0.001;OS:log-rank p<0.001)。
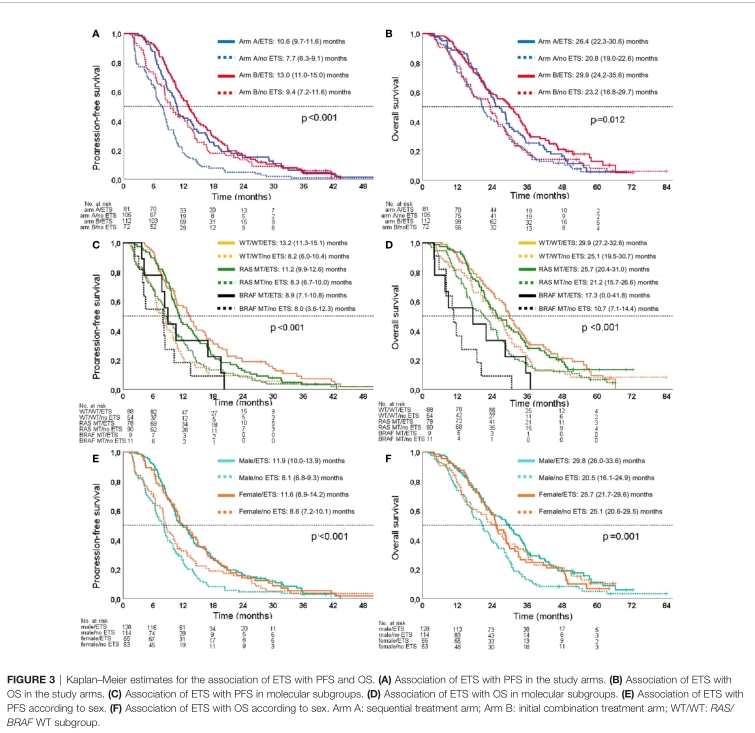
男性患者中,ETS与PFS[log rank p<0.001;HR 0.532 95% CI 0.409-0.692)和OS [log rank p<0.001;HR 0.574 95%CI 0.437-0.756)]相关。然而,这种相关性在女性患者无相关性。当对治疗组、年龄、RAS突变和BRAF突变的预测效果进行调整时,这些性别差异也很明显[男性PFS:p<0.001,HR 0.550 (95%CI 0.418-0.725);女性PFS: p = 0.109, HR 0.734 (95% CI 0.503-1.072);男性OS:p = 0.001, HR 0.617 (95% CI 0.465-0.891);OS女性:p = 0.490, HR 0.868 (95% CI 0.581-1.297)]。
综上,研究表明,初始贝伐珠单抗联合治疗可改善转移性结直肠癌(mCRC)患者的ETS 和DpR。ETS可作为其预后指标。
原始出处:
Kurreck A, Heinemann V,Fischer von Weikersthal L, et al (2022) Response and Disease Dynamics in Untreated Metastatic Colorectal Cancer With Bevacizumab-Based Sequential vs. Combination Chemotherapy—Analysis of Phase 3 XELAVIRI Trial. Front. Oncol. 12:751453.doi: 10.3389/fonc.2022.751453.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#III期临床研究#
51
#I期临床#
47
#Oncol#
59
#II期临床研究#
55
#CRC#
41
#mCRC#
38
#III#
40
#贝伐珠#
42
贝伐珠单抗在转移性结直肠癌中的地位依然如故
49
#联合治疗#
37