J Endod:Toll-like受体2/IL-10双敲小鼠内牙髓感染导致的炎症与颌骨骨髓炎相似
2019-02-18 lishiting MedSci原创
一般来讲,小鼠牙髓感染后会导致慢性不愈合的尖周损伤。令人惊奇的是,作者近日研究发现,Toll-like受体2(TLR2)/IL-10双敲(dKO)小鼠展现出急性但可治愈的骨髓炎样炎症反应。为此,这篇研究的目的是为了检测TLR2/IL-10 dKO小鼠牙髓感染引起的炎症变化以及探索缺氧诱导因子(HIF-1α)亚基和精氨酸酶1介导的尖周损伤愈合的潜在机制。
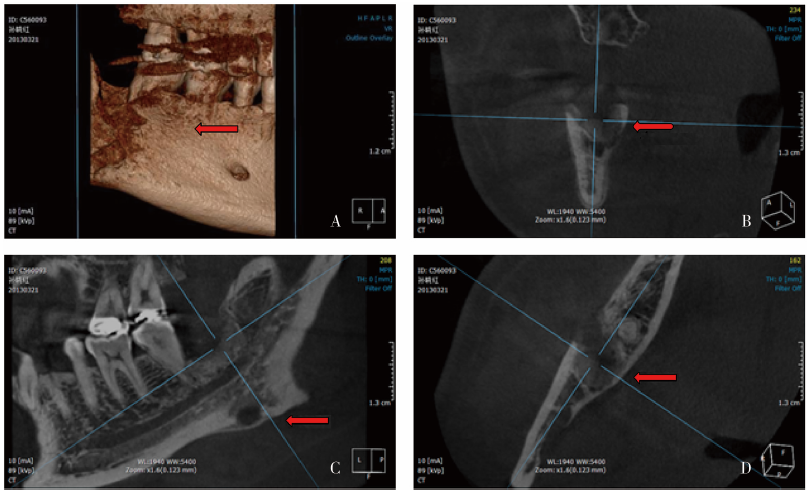
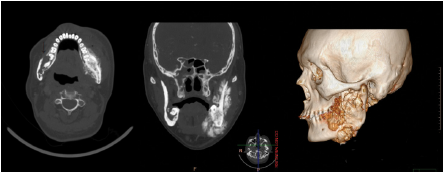
一般来讲,小鼠牙髓感染后会导致慢性不愈合的尖周损伤。令人惊奇的是,作者近日研究发现,Toll-like受体2(TLR2)/IL-10双敲(dKO)小鼠展现出急性但可治愈的骨髓炎样炎症反应。为此,这篇研究的目的是为了检测TLR2/IL-10 dKO小鼠牙髓感染引起的炎症变化以及探索缺氧诱导因子(HIF-1α)亚基和精氨酸酶1介导的尖周损伤愈合的潜在机制。研究对TLR2/IL-10 dKO和野生型C57BL/6J小鼠的下颌第一磨牙制备牙髓感染。小鼠在感染后的days 0 (noninfected), 10和21处死。分别通过micro-CT、组织学、骨多彩标记和microarray分析检测骨组织破坏程度、炎症水平、骨沉积和基因表达变化。另外,通过在感染TLR2/IL-10 dKO小鼠内使用特异性抑制剂YC-1,检测阻断内源性HIF-1α的作用。结果显示, TLR2/IL-10 dKO小鼠在感染后10天展现出广泛的骨组织破坏和炎症反应,在感染后21天出现自发性的尖周损伤愈合,包括:骨形成和炎症消退。相反,WT小鼠在21天的观察期间展现出持续增加的慢性尖周炎症反应。基因表达分析和免疫组化显示,
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Toll-like#
32
#牙髓#
32
#牙髓感染#
39
#骨髓炎#
37
#IL-1#
37
#IL-10#
44
学习了,谢谢分享
0