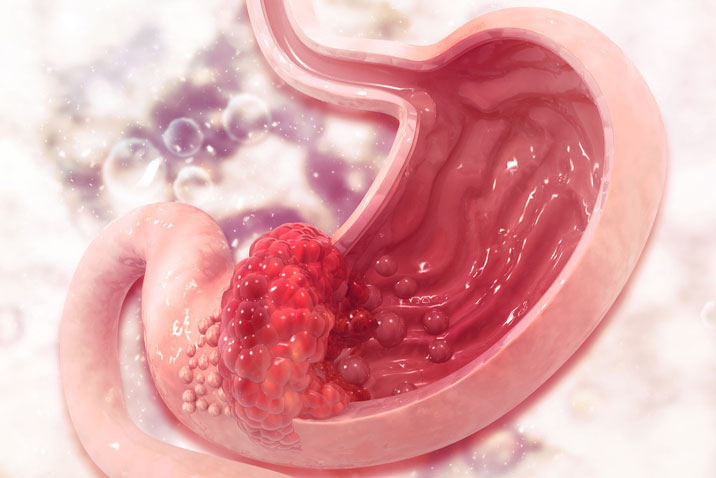
JAMA Surg:腹腔镜vs机器人胃切除术对胃癌患者短期预后的影响
2021-09-03 MedSci原创 MedSci原创
对于准备接受胃癌切除术的患者,与传统的腹腔镜胃切除术相比,机器人胃切除术并没有减少术后患者腹腔内感染性并发症风险,但总不良事件风险降低

微创手术,以腹腔镜手术为代表,广泛用于胃癌(GC)的治疗。若干多中心随机临床试验(RCTs)报道称,与开放式胃切除术相比,腹腔镜胃切除术(LG)患者术后并发症风险较低,但两者长期预后差异不显著。近年来,机器人胃切除术(RG)的使用率不断增加,有研究称RG在降低腹腔内感染并发症风险方面具有优势。近日研究人员比较了胃癌患者接受机器人胃切除术或腹腔镜胃切除术对短期预后的影响。
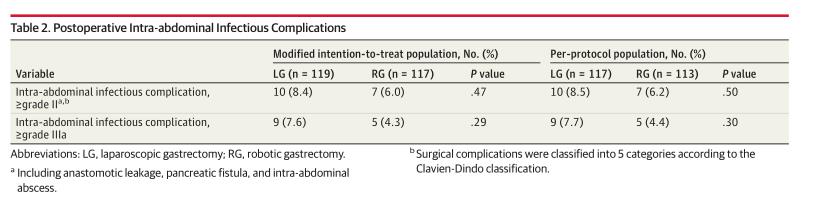
本次研究为III期研究,241名临床分期为I-III期的可手术胃癌患者参与,随机接受LG或RG,研究的主要终点是术后腹腔内感染并发症的发生率。次要终点是任何并发症的发生率、手术结果、术后病程和肿瘤学结果。
241名患者中,122名被随机分配到LG组,119名患者被随机分配到RG组。LG组患者中有2名(1.6%)从LG转为开放手术,RG组患者中有4名(3.4%)从RG转为开放或腹腔镜手术。最后,LG组117名患者完成了手术,RG组113名患者完成了手术,其中150名男性,平均年龄70.8岁。组间腹腔内感染并发症的发生率没有显著差异(LG组117例患者中的10例[8.5%]出现腹腔内感染并发症,RG组113例患者中有7例[6.2%])。LG组术后II级或以上并发症的总发生率为19.7%,显著高于RG组的8.8%。即使在仅限于IIIa级或更高级别的不良事件分析中,LG组的并发症发生率仍显著高于RG组(16.25% vs5.3%)。
研究认为,对于准备接受胃癌切除术的患者,与传统的腹腔镜胃切除术相比,机器人胃切除术并没有减少术后患者腹腔内感染性并发症风险,但总不良事件风险降低。
原始出处:
Toshiyasu Ojima et al. Short-term Outcomes of Robotic Gastrectomy vs Laparoscopic Gastrectomy for Patients With Gastric Cancer A Randomized Clinical Trial. JAMA Surg. September 1, 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#胃癌患者#
37
#切除术#
36
#腹腔镜#
42
#机器人#
35
#胃切除#
42
#机器#
39
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
55