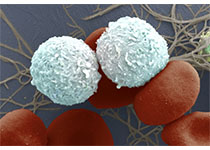
AGING CELL:活性氧诱导衰老肝脏中的胆固醇积累
2019-01-05 海北 MedSci原创
老龄化是许多慢性病的主要危险因素,因为衰老个体对外部压力的易感性增加,并且易患疾病。已有的研究也显示,衰老与代谢性肝病,如非酒精性脂肪肝,有关。
老龄化是许多慢性病的主要危险因素,因为衰老个体对外部压力的易感性增加,并且易患疾病。已有的研究也显示,衰老与代谢性肝病,如非酒精性脂肪肝,有关。
最近,研究人员探究了小鼠衰老过程中脂质代谢的变化及其相关机制。老年小鼠肝组织中脂质积累增加,尤其是胆固醇。与年轻小鼠相比,在老年小鼠的肝细胞中观察到胆固醇和葡萄糖的摄取增加。在衰老过程中,用于胆固醇合成的GLUT2,GK,SREBP2,HMGCR和HMGCS的mRNA表达在肝组织中逐渐增加。
活性氧(ROS)随着衰老而增加,并且与各种和衰老有关的疾病密切相关。当研究人员用ROS诱导剂H2O2处理HepG2细胞和原代肝细胞时,与未处理的HepG2细胞相比,脂质积累显着增加。 H2O2处理显着增加葡萄糖摄取和乙酰辅酶A产生,这导致糖酵解和脂质合成的发生。用H2O2处理显着增加了与胆固醇合成和摄取相关的基因的mRNA表达。
这些结果表明,ROS在改变胆固醇代谢中起重要作用,因此在衰老过程中加剧肝脏中胆固醇的积累。
原始出处:
Eunhui Seo et al. Reactive oxygen species‐induced changes in glucose and lipid metabolism contribute to the accumulation of cholesterol in the liver during aging. AGING CELL, 2018; doi: https://doi.org/10.1111/acel.12895
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Cell#
23
#CEL#
37
#活性氧#
39
学习了,涨知识了!
55