Invest Ophthalmol Vis Sci:深度学习的神经网络算法检测视网膜病变!
2018-01-31 cuiguizhong MedSci原创
美国加利福尼亚州圣何塞市圣克拉拉谷医疗中心眼科和斯坦福大学生物医学数据科学系的Lam C近日在Invest Ophthalmol Vis Sci发表了一项重要的工作,他们开发了一种自动化的方法来定位和辨别视网膜图像中的多种类型的特征。这套方法使用有限的数据进行训练,中间没有编码特征提取的算法。因为有的疾病的数据有限,所以可以将此算法推广到少数疾病检测的步骤中。
美国加利福尼亚州圣何塞市圣克拉拉谷医疗中心眼科和斯坦福大学生物医学数据科学系的Lam C近日在Invest Ophthalmol Vis Sci发表了一项重要的工作,他们开发了一种自动化的方法来定位和辨别视网膜图像中的多种类型的特征。这套方法使用有限的数据进行训练,中间没有编码特征提取的算法。因为有的疾病的数据有限,所以可以将此算法推广到少数疾病检测的步骤中。
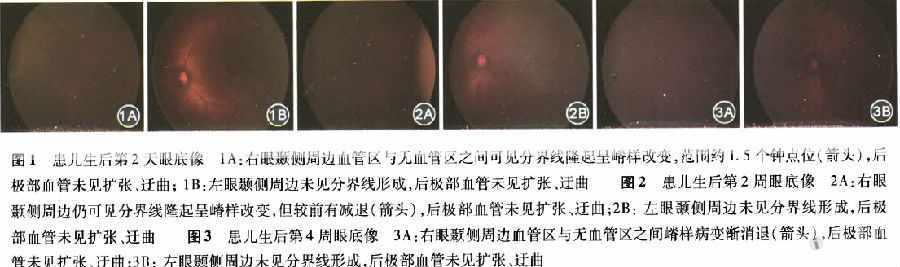
两名眼科医生诊断了243幅视网膜图像,标记图像的重要部分,产生了1324个图像块,得到包含出血、微动脉瘤、渗出物、视网膜新血管形成或来自Kaggle数据集的正常结构等。用这些图像块来训练一个标准的卷积神经网络,达到可以预测上述五个类别。

他们使用该方法在eOphta数据库上验证了148个全视网膜微动脉瘤图像和47个分泌物。在0.94和0.95的ROC曲线下面积的像素分类得到微动脉瘤和分泌物,在0.86和0.64的精确回忆曲线下得到病灶面积。
因此,他们认为,区域训练的卷积神经网络可以产生病变特异性的概率图,能够检测和区分微妙的病理损伤,而这样的预测结果只需要每个损伤几百个训练样本就可以达到。
原文出处:
Lam, C., et al., Retinal Lesion Detection With Deep Learning Using Image Patches. Invest Ophthalmol Vis Sci, 2018. 59(1): p. 590-596.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#EST#
24
#神经网络算法#
31
henhao
60
学习了不少事情!!
63
#神经网络#
29
#THA#
25
#视网膜病变#
25
#视网膜#
30
谢谢了.学习
65
学习了新知识
70