Circ: Cardiovascular Interventions:左束支传导阻滞对经导管主动脉瓣置换术的影响
2018-11-20 xiangting MedSci原创
先前存在LBBB显著增加TAVR后早期PPI的风险(而不是晚期),对总体死亡率或心血管死亡率没有任何显著影响。
先前存在的左束支传导阻滞(LBBB)对经导管主动脉瓣置换术(TAVR)受者的影响尚不清楚。这项研究目的是确定先前存在的LBBB对TAVR后临床结局的影响。
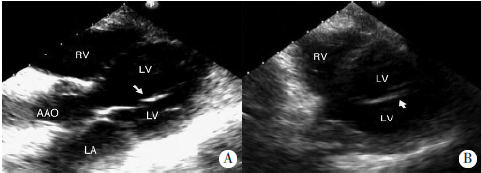
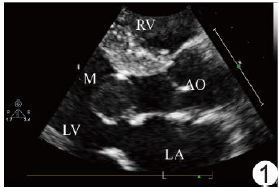
这项多中心研究根据基线ECG是否存在LBBB,评估了3404名TAVR候选者。根据瓣膜学术研究联盟-2定义了TAVR并发症和死因。在30天、12个月和此后每年进行门诊随访或电话访问。在基线、出院时和1年随访时进行超声心动图检查。398名患者(11.7%)先前存在LBBB,并与永久起搏器植入风险升高相关(PPI; 21.1% vs 14.8%;调整后的比值比,1.51; 95%CI,1.12-2.04),但与30天死亡率不相关(7.3%vs 5.5%;调整后的比值比,1.33; 95%CI,0.84-2.12)。平均随访22±21个月,先前存在和不存在LBBB患者的总体死亡率(校正风险比,0.94; 95%CI,0.75-1.18)和心血管死亡率无差异(校正风险比,0.90; 95%CI,0.68-1.21)。在对2421名无PPI患者进行PPI 30天和完全随访的亚组分析中,先前存在LBBB与PPI或心源性猝死的风险升高无关。先前存在LBBB患者在基线和1年随访时左心室射血分数(LVEF)较低(P均<0.001),但与先前不存在LBBB的患者相比,LVEF低的患者TAVR后的LVEF随时间有相似升高(P=0.327)。
先前存在LBBB显著增加TAVR后早期进行PPI的风险(而不是晚期),对总体死亡率或心血管死亡率没有任何显著影响。先前存在LBBB与TAVR前较低的LVEF相关,但与无LBBB患者相似,先前存在LBBB并不阻止TAVR后LVEF的升高。
原始出处:
Quentin Fischer. Impact of Preexisting Left Bundle Branch Block in Transcatheter Aortic Valve Replacement Recipients. Circ: Cardiovascular Interventions. 19 November 2018.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#左束支传导阻滞#
28
#置换#
27
#ASC#
25
#vascular#
25
#传导阻滞#
31
#主动脉瓣#
32
#主动脉瓣置换术#
33
#主动脉#
0
#cardiovascular#
47
#经导管#
30