Ther Adv Med Oncol:北京协和医院团队真实世界探索HER2改变的晚期NSCLC患者更佳一线治疗方案
2022-03-11 yd2015 MedSci原创
研究表明,晚期HER2改变的NSCLC患者中化疗联合抗血管生存治疗可能更优。
近期,Therapeutic Advances in Medical Oncology杂志上发表了一项来自北京协和医院团队的回顾性真实世界研究成果,主要是探索HER2改变的晚期NSCLC患者中,以化疗为基础的最佳一线治疗方案。
研究纳入2015年11月至2021年9月期间接受一线治疗的HER2改变的晚期NSCLC患者。根据患者治疗手段分为:接受化疗单药(C)、化疗联合免疫治疗(C+I)或化疗联合抗血管生成治疗(C+A)。比较亚组间的无进展生存期(PFS)。
研究总共筛选了293例患者,鉴定出HER2扩增和37个不同的HER2突变,最常见的变异亚型为20外显子插入(ex20ins, n= 246,83.9%);其中,A775_ G776insYVMA的 12 bp插入 (n=166, 56.7%)最多,其次是G776delinsVC的6 bp插入 (n=30, 10.2%)、P780_Y781insGSP的9 bp插入 (n=29, 9.8%)和其他ex20ins变异体(n=21, 7.2%)。
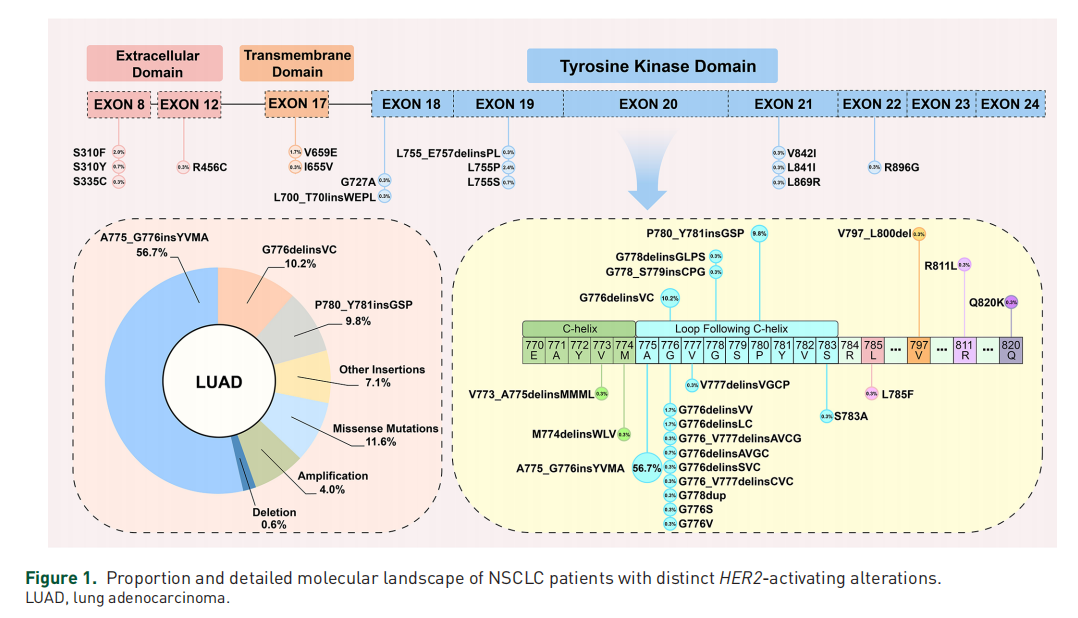
KEGG分析显示,PI3k /AKT信号通路在HER2改变的NSCLC中普遍上调。
最终纳入了210例一线以化疗为基础的患者,其中C、C+I或C+A治疗患者分别为83(39.5%), 81 (38.6%), 和 46(21.9%)例。C组的ORR、DCR、中位PFS和中位OS分别为16.9%(14/83)、89.2%(74/83)、4.03个月(95% CI: 2.70 -5.37)和31.67个月(95% CI: 29.63-33.71)。C+A组的ORR、DCR、中位PFS和中位OS分别为23.8%(19/80)、91.3%(73/80)、5.63个月(95% CI: 4.84-6.43)和36.27个月(95% CI: 28.71-42.83)。C+I组的ORR、DCR和中位PFS分别为28.9%(13/45)、80.0%(36/45)和5.20个月(95% CI: 3.64 6.76)。中位OS尚未成熟,其中6个月和12个月生存率分别为75.6%(34/45)和53.3%(24/45)。
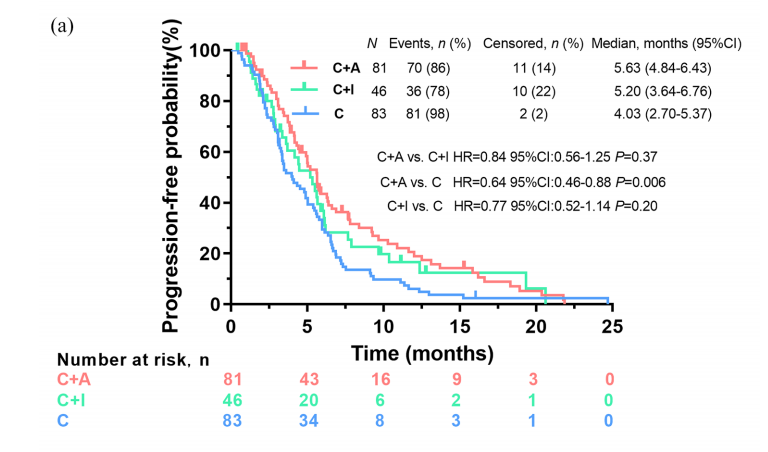
C+A和C亚组之间观察到显著的PFS差异(中位数,5.63 vs 4.03个月,HR=0.64, 95% CI: 0.46-0.88, p=0.006)。C+I亚组和C亚组之间PFS无统计学差异(中位数,5.20 vs 4.03个月,HR=0.77, 95% CI: 0.52-1.14 p=0.20),或C+A和C+I亚组之间无差异(中位数,5.63 vs 5.20个月,HR=0.84, 95% CI: 0.56-1.25, p=0.37)。C+A和C的OS无差异(中位数,36.27 vs 31.67个月,HR=1.07, 95% CI: 0.64-1.78, p=0.80)。
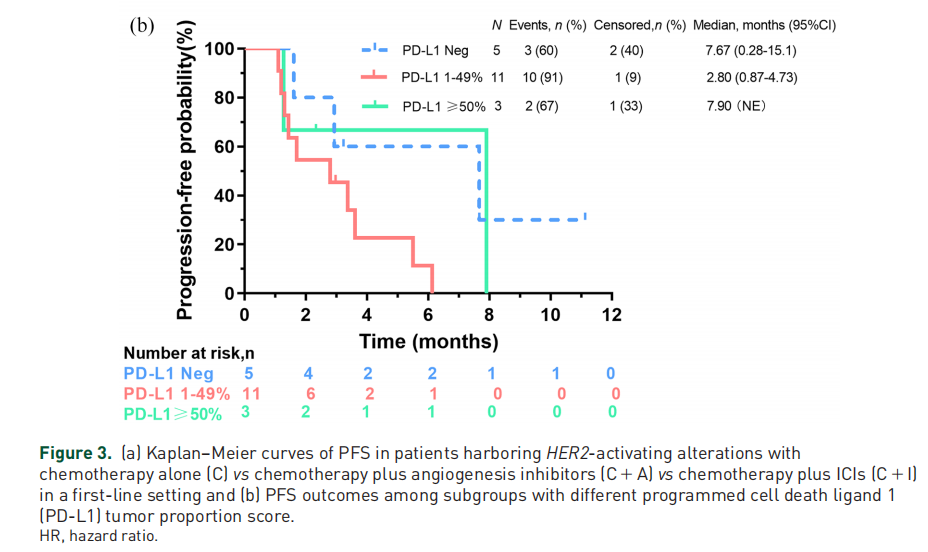
19例获得PD-L1表达状态患者中,5例TPS阴性患者的ORR为20%(1/5),中位PFS为7.67个月(95% CI: 0.28 -15.1)。在11例TPS为1-50%的患者中,ORR为18.2%(2/11),中位PFS为2.80个月(95% CI: 0.87-4.73)。值得注意的是,在3例TPS≧50%的患者中(2例TPS为50%,1例TPS为95%),只有1例达到PR, PFS为2.33个月。其中一名患者达到SD,无进展生存期为7.90个月,另一名患者在初始反应评估时发展为PD,无进展生存期为1.27个月。
综上,研究表明,晚期HER2改变的NSCLC患者中化疗联合抗血管生存治疗可能更优。
原始出处:
Yang G, Yang Y, Liu R, Li W, Xu H, Hao X, Li J, Xing P, Zhang S, Ai X, Xu F, Wang Y. First-line immunotherapy or angiogenesis inhibitor plus chemotherapy for HER2-altered NSCLC: a retrospective real-world POLISH study. Ther Adv Med Oncol. 2022 Mar 2;14:17588359221082339. doi: 10.1177/17588359221082339. PMID: 35251321; PMCID: PMC8894956.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#北京协和医院#
41
#治疗方案#
65
#北京协和#
41
#Oncol#
24
#SCLC患者#
31
#真实世界#
34
#协和#
31
#NSCLC患者#
40
#晚期NSCLC#
36
#协和医院#
36