标本采集是医务人员的日常工作之一,采集行为直接影响检验科收到的标本状态,进而影响医生对病情的判断和疾病诊治。血标本采集的正确与否及其质量好坏直接影响到检验结果的准确性,进而影响临床诊断。一个有价值的检验结果需要护理人员、患者、检验人员多方面的密切配合才能完成。
现就检验人员在采取血标本中常遇到的不合格标本原因及对策做总结:
血液标本不合格原因
1、标本凝块:
2、标本量少:
3、采血管出现错误: 在采血过程中使用了不正确的采血管;
4、真空采血管出现破损;
5、血样送检时间超时。未按照相关规定将采集到的血样送到相应检验室;
6、血样标本信息存在错误或者没有检测的项目要求;
7、没有采集到血样标本;
8、出现溶血问题,如重度或者重度溶血;
9、严重脂血,主要呈现为牛奶状;
10、采集到的血样标本受到污染,如运送中没有加盖导致被其他的标本污染。
检验科室凡是遇到上述任何的一个情况都将血标本判定为不合格标本,会立即致电病区护士,核对患者的信息、不合格原因等,并在做出判断后要求临床护士重新采血。
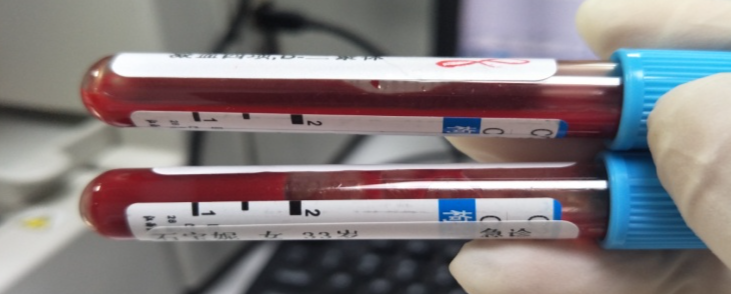
在临床工作中,遇到最多的不合格标本还是溶血和凝血。凝血分为肉眼不容易发现的血凝块及是液凝固两种类型。导致出现这两种现象的原因主要是:在对患者进行抽血的时候不顺利,抽血时间过长。这样操作带来的问题是血液可能在针管当中已经出现凝固;或在血液被注入到针管当中的时候,没有立即轻摇,从而也可能造成部分的血液凝集;或在进行摇晃的时候,摇晃不均匀,时间不够充分,使得血液没有和抗凝剂充分混合;其次就是采血量不足或者是操作不规范的问题。

标本溶血原因
1、病人血管不充盈,用止血带时间过长,捆扎过紧,并反复用力拍打穿刺部位,引起血管内溶血;
2、穿刺不顺利,针尖在静脉中反复探寻,损伤组织过多,造成血肿而溶血:
3、混匀抗凝管时用力过猛或送检时振荡过大;
4、从已有血肿的静脉采血,血样可能含有已溶血的细胞;
5、未使用采血针,而使用了一次性注射器,抽血过快,采血后将血从注射器注入试管过猛,血细胞受外力而溶血;
6、标本量不足,血液和抗凝剂比例失调,由于渗透压的改变发生溶血;
7、静脉穿刺处用酒精或碘伏消毒,酒精或碘伏未干即开始采血;
8、注射器或盛血容器不干燥或容器污染;
9、注射器和针头连接不紧,采血时空气进入,产生气泡,发生溶血;
10、用真空管采血却未抽足量,即真空管内还残留部分负压,引起标本溶血。
对策
1、按顺序采血,多管采血时的采血顺序为:血培养、不含添加剂的采血管(血清标本管,红色、桔红色或黄色)、凝血标本管(浅蓝色)、其他标本管。
2、规范标本采集方法,使用真空采血器,尽量不用注射器采血:
3、真空管采血不足时,应开盖平衡试管内外压力,然后再盖上;
4、避免不合格的采血器具,勿用过细的针头,抽吸不要用力过猛过快,不要从血肿处采血;
5、选择正确的采血时间及体位, 一般选择清晨空腹时卧位采血;
6、采血部位:临床采血部位多用肘正中静脉或贵要静脉,不能选择过细的静脉, 否则血量不足, 导致溶血;
7、标本采集后应迅速送到检验室, 防止标本中某些成分的降解。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#不合格#
35
#标本#
40
#血液标本#
48
#标本采集#
37