JAMA:中国城乡糖尿病患病率及死亡率
2017-01-18 医咖会 医咖会
2017年1月17日,JAMA刊登了中国慢性病前瞻性研究(China Kadoorie Biobank, CKB)项目的一项研究进展,公布了中国城乡糖尿病患病率及死亡率的数据。该研究的通讯作者为英国牛津大学的陈铮鸣教授和北京大学公共卫生学院的李立明教授。 近几十年来,中国糖尿病患病率大幅增加,但是目前还缺乏糖尿病相关的超额死亡率的可靠数据。本研究对中国农村和城市地区的糖尿病相关超额死亡率进行
2017年1月17日,JAMA刊登了中国慢性病前瞻性研究(China Kadoorie Biobank, CKB)项目的一项研究进展,公布了中国城乡糖尿病患病率及死亡率的数据。该研究的通讯作者为英国牛津大学的陈铮鸣教授和北京大学公共卫生学院的李立明教授。
近几十年来,中国糖尿病患病率大幅增加,但是目前还缺乏糖尿病相关的超额死亡率的可靠数据。本研究对中国农村和城市地区的糖尿病相关超额死亡率进行了评估。
这是一项持续7年的全国前瞻性研究,涉及中国的10个地区(5个农村+5个城市),在2004年6月到2008年7月,共纳入30-79岁的512869名成年人,随访至2014年1月。
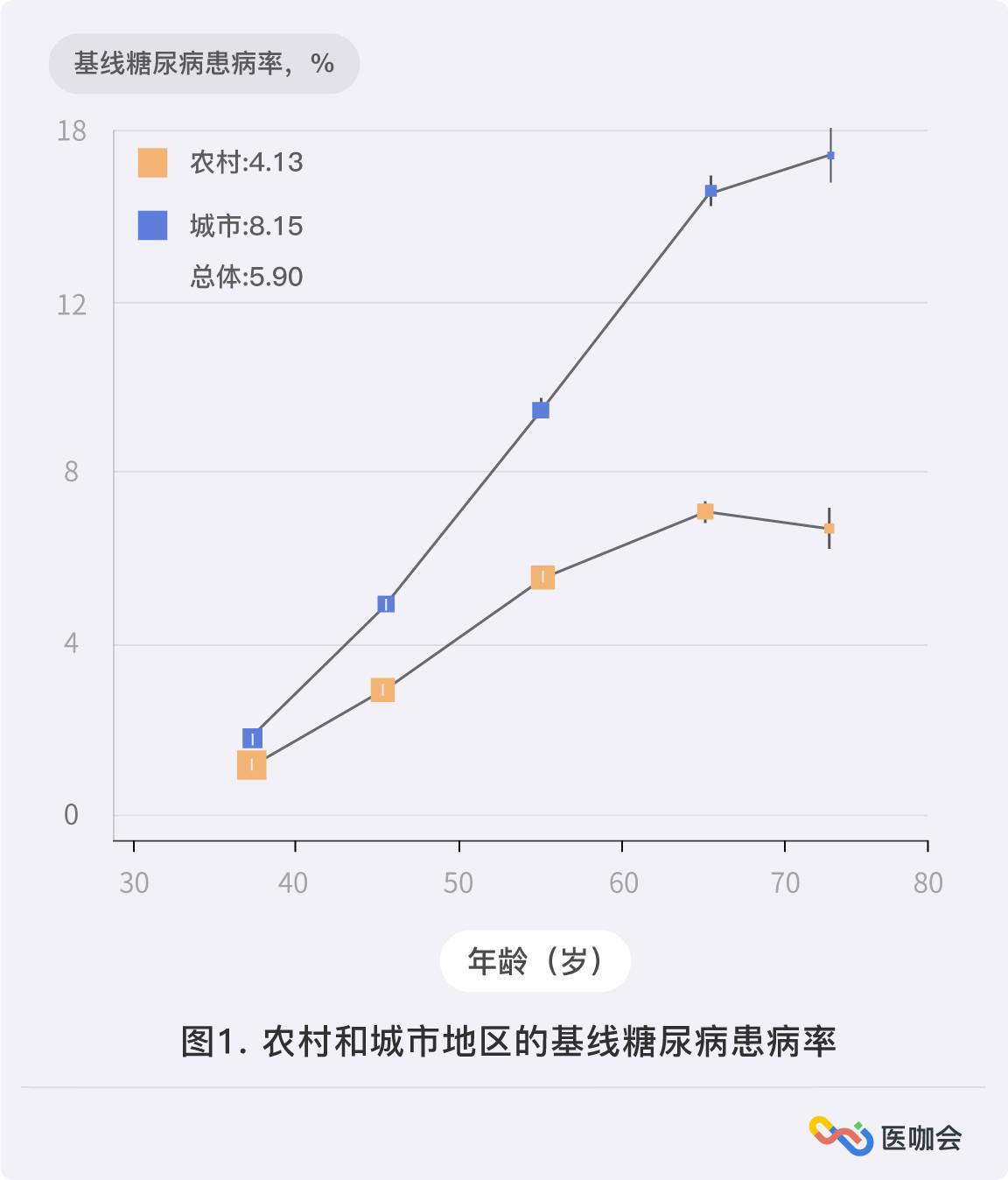
512869名参与者的平均年龄为51.5岁,其中59%是女性。结果发现,5.9%(n=30280)的人患有糖尿病。农村地区的糖尿病患病率为4.1%,城市地区为8.1%;男性的糖尿病患病率为5.8%,女性为6.1%。
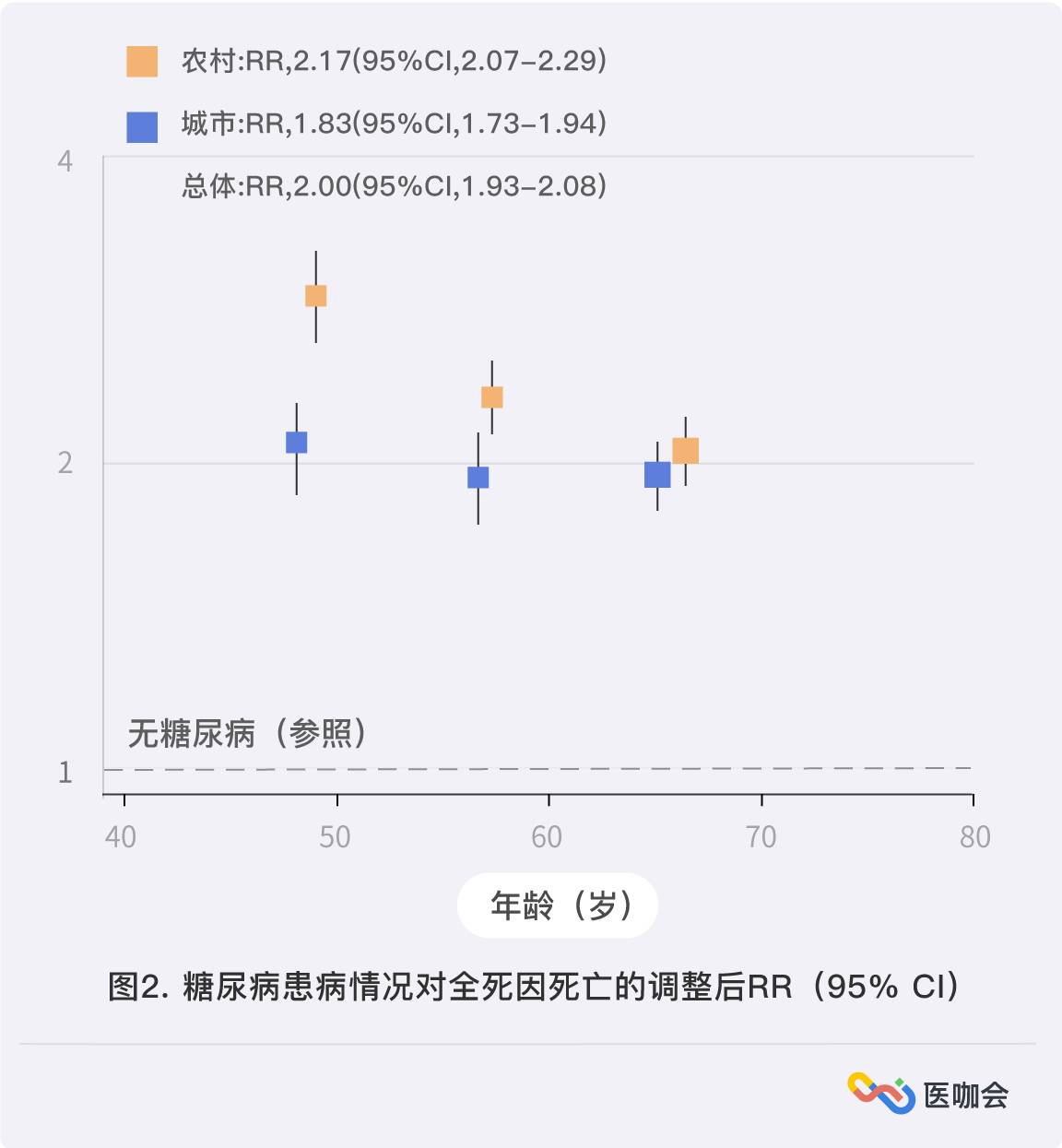
共随访364万人年,有24909例死亡,其中3384例为糖尿病患者。与无糖尿病人群相比,糖尿病患者的全死因死亡率显著增加[1373/10万人 vs 646/10万人;调整RR,2.00(95%CI, 1.93-2.08)],农村地区要高于城市地区(农村地区RR=2.17;城市地区RR=1.83)。(图1、图2)
糖尿病与下列疾病的死亡率增加有相关性:心血管疾病(RR=2.13),包括缺血性心脏病(RR=2.40),卒中(RR=1.98)。慢性肝病(RR=2.32),感染(RR=2.29)。肝癌(RR=1.54),胰腺癌(RR=1.84),女性乳腺癌(RR=1.84),女性生殖系统肿瘤
(RR=1.81)。糖尿病与肺癌、胃癌和结直肠癌死亡率的升高无关。(表1)
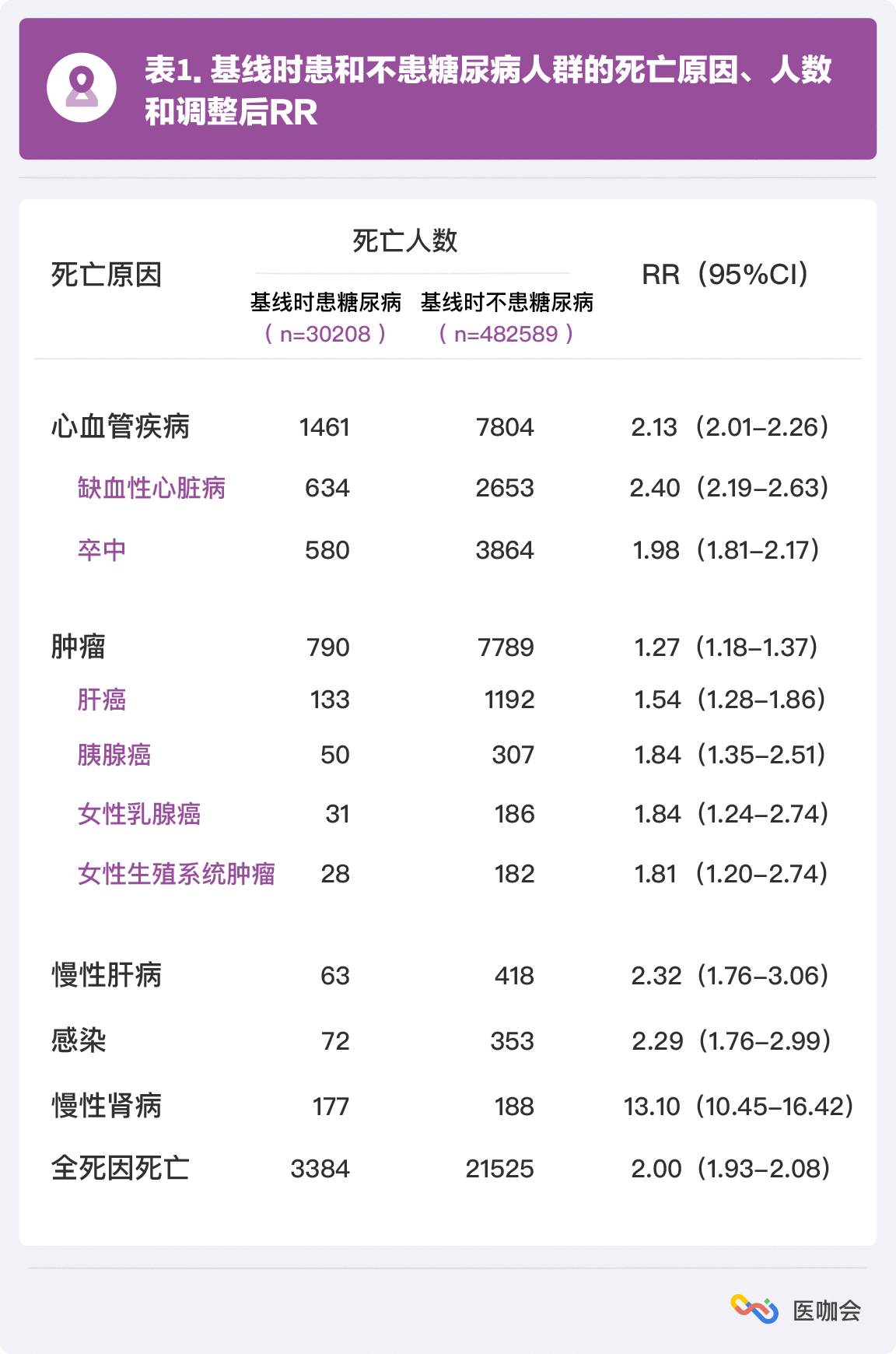
糖尿病与慢性肾病的死亡率增加有相关性(RR=13.10),其中糖尿病肾病的RR最高,达到83.29。相比城市地区(RR=6.83),农村地区的糖尿病患者因慢性肾病的死亡率更高(RR=18.69)。糖尿病患者中,10%的死亡(农村为16%,城市为4%)是由于(确定或怀疑)糖尿病酮症酸中毒或昏迷造成的(408例死亡)。
研究得出结论:中国成年人中,糖尿病与很多心血管和非心血管疾病死亡率增加具有相关性。虽然城市地区的糖尿病患病率更高,但是农村地区糖尿病的超额死亡率更大。
原始出处:
Fiona Bragg, DPhil1; Michael V. Holmes, PhD1,2; Andri Iona, MSc1,2; et al.Association Between Diabetes and Cause-Specific Mortality in Rural and Urban Areas of China.JAMA. 2017;317(3):280-289. doi:10.1001/jama.2016.19720
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












发病率还是挺高的
64
#患病率#
27
重量级临床文章
88
新想法的
57
李立明教授好牛
62
发人深省
60
棒棒哒????
19
谢谢作者,谢谢科研人员!
20
怎么只有标题?!
25
学习啦,谢谢分享
29