AACR 2020:卡瑞利珠单抗+阿帕替尼治疗SCLC(小细胞肺癌)的II期研究
2020-04-28 MedSci MedSci原创
卡瑞利珠单抗和阿帕替尼分别为恒瑞医药研发的PD1单抗和口服抗血管多靶点TKI,双药组合在多个癌种都在火热进行研究,初步数据非常亮眼,并且做到了无化疗!
卡瑞利珠单抗和阿帕替尼分别为恒瑞医药研发的PD1单抗和口服抗血管多靶点TKI,双药组合在多个癌种都在火热进行研究,初步数据非常亮眼,并且做到了无化疗!
一项由王洁教授团队进行的研究纳入了2018年4月-2019年3月期间的59例既往铂类耐药的广泛期SCLC患者,随机分为阿帕替尼 375mg每日服用组,5天连服后停两天组和连服7天停7天组。卡瑞利珠单抗均为200mg/2周。在AACR 2020大会上公布结果。
结果显示,在阿帕替尼每日连服组中,ORR(客观缓解率)达到了34%,中位PFS(无进展生存期)为3.6个月,中位OS(总生存期)为8.4个月。无论患者既往对化疗敏感(≥90天后复发)或抵抗(<90天内复发),ORR都不错(37.5% vs 32.3%),中位PFS为3.6 vs 2.7个月,中位OS为9.6 vs 8个月。治疗相关3级及以上AE发生率为72.9%。总体不良反应可管理。
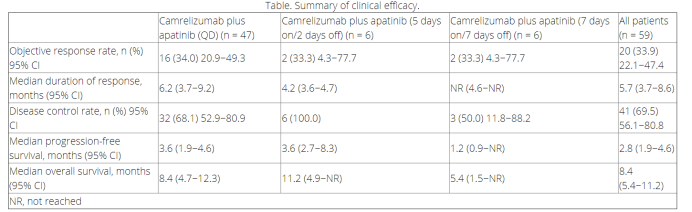
对于化疗后进展的SCLC患者,预后并不佳。恒瑞PD1+阿帕替尼在后线治疗仍可以达到34%的ORR级8.4个月的OS,已经是超越了现有所有标准治疗的疗效。并且,这两种药物目前国内都已经上市,药物可及,名副其实的给SCLC患者提供了高效的无化疗方案。
梅斯医学研究员李博士评论道,Durvalumab联合化疗用于SCLC时,中位总生存期(OS)是13.0月,而标准治疗组是10.3月,相比而言,延长了3个月。同样,Tecentriq(atezolizumab)联合化疗(卡铂+依托泊苷),用于一线治疗广泛期小细胞肺癌(ES-SCLC)成人患者。与化疗相比,Tecentriq+化疗方案显著延长了总生存期(中位OS:12.3个月 vs 10.3个月),约2个月左右。但是,本例选择的是既往铂类耐药的广泛期SCLC患者,这类患者预后更差,与标准治疗相比,中位OS达到8.4个月,是一个相当不错的结果。
在SCLC这个细分领域,几个重要的免疫治疗药物可能会面临激烈的竞争。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#AACR 2020#
31
#卡瑞利珠单抗#
122
#ACR#
34
#卡瑞利珠#
33
#AACR#
24