Nat Commun:侵袭性前列腺癌中的内含子保留和剪接体研究
2020-05-14 AlexYang MedSci原创
mRNA可变剪接(AS)的异常调控在实体瘤发展和进展中的作用仍旧不确定。
mRNA可变剪接(AS)的异常调控在实体瘤发展和进展中的作用仍旧不确定。
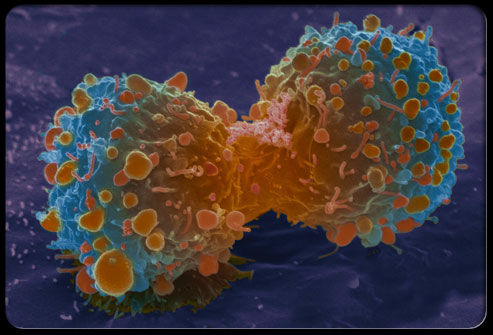
最近,有研究人员首次综合性的描述了人类前列腺癌(PCa)进化过程中的AS情况。研究人员发现,剪接异常调控的严重度与疾病进展有关,并提出内含子保留是PCa干细胞华和侵袭性的一个标志。对274个剪接调控基因(SRGs)的系统性调查发现了普遍存在的基因组拷贝数变异(CNVs),导致了PCa发展和恶化过程中大约68%的SRG基因异常表达。因此,许多SRGs是具有预后性质的。令人惊讶的是,雄激素受体能够控制剪接过程,且与其转录调控不同。在异种种植模型和原生PCa模型中,剪接体调控因子E7107能够逆转癌症恶化并抑制趋势抵抗性PCa(CRPC)。
最后,研究人员指出,他们的结果建立了由SRGs异常调控引起的异常AS情况,并且是PCa侵袭性的一个标志,剪接体可作为CRPC的治疗靶标。
原始出处:
Cheng Liu, Li Liu, Kun Wang et al. VHL-HIF-2α axis-induced SMYD3 upregulation drives renal cell carcinoma progression via direct trans-activation of EGFR. Oncogene. 14 April 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#剪接体#
40
#COMMUN#
33
#Nat#
0
#内含子保留#
27
#侵袭性#
33
非常好的文献
74
前列腺癌相关研究,学习了,谢谢梅斯
43