【一般资料】
患者,女,68岁。
【现病史】
因跌倒致右肘关节损伤,于外院行X线片检查示:右肘关节脱位并尺骨近端、桡骨头骨折。外院行手法复位术治疗后,肘关节不稳、活动受限,于伤后6个月入我院治疗。
【体格检查】
右肘侧方外翻不稳并后脱位,屈伸活动度为20°~70°,前臂旋前活动度约为50°,旋后活动度约为60°,右上肢肌力、感觉正常。
【辅助检查】
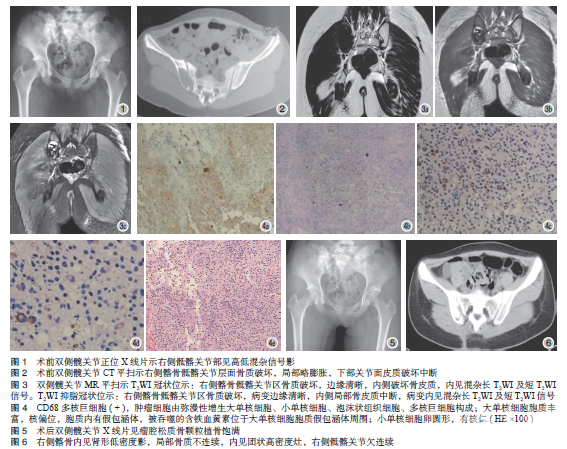
X线片及CT检查示:右肘关节后脱位,右尺骨冠状突骨折(Regan&MorreyⅢ型),右桡骨小头骨折(MasonⅣ型,见图1)

【初步诊断】
侧陈旧性肘关节脱位。
【治疗】
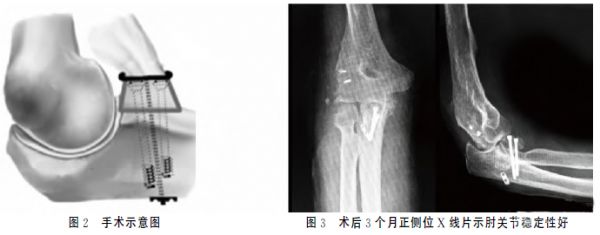
臂丛神经阻滞麻醉下患者取平卧位,驱血、上气压止血带。作肘关节外侧切口,显露肱骨外髁、桡骨小头,见桡骨小头陈旧性骨折,用微型摆锯清除桡骨头关节面增生骨赘,清理瘢痕组织后行肘关节拔伸牵引及松解术。探查见尺骨冠状突骨折块位于肘关节内侧被瘢痕包裹,作肘关节前内侧切口,取出冠状突骨折块,骨折块粉碎变薄,难以将其修复固定,且手法复位肘关节后,肘关节不稳定,屈伸即刻发生后脱位。局麻下于右侧髂前上棘凿取1块髂骨块,将骨块修整成合适大小,带骨膜的骨面朝向肱骨滑车关节面植入冠状突缺损处,以2枚克氏针做临时固定后,拧入2枚3.0MM空心钉固定。用不可吸收缝线缝合前关节囊,从尺骨背侧向移植的自体髂骨钻入带孔克氏针作一隧道,将不可吸收缝线经带孔克氏针穿过骨隧道;取AO手指钢板修剪成2孔小钢板,将穿过骨隧道的缝线绑扎于小钢板上,固定于尺骨背侧皮质。最后以带线锚钉修复肘关节外侧副韧带(见图2)。检查肘关节屈曲活动良好、无后脱位、前臂旋转稳定后,分层缝合,留置引流管,加压包扎。予屈肘90°、前臂中立位石膏托外固定。术后处理 术后1周进行肱二头肌及肱三头肌等长收缩训练;术后3周拆除石膏托,在肘关节支具保护下行肘关节屈伸和前臂旋转功能锻炼,支具活动范围设定在50°~110°;术后6周拆除外固定支具,开始非限制性肘关节屈伸及前臂旋转功能锻炼。结果术后3个月X线片复查示尺骨冠状突骨性愈合。12个月随访时,肘关节活动度为:屈伸30°~110°,前臂旋前70°、旋后75°;肘关节稳定性好,未再发生后脱位;Morrey肘关节功能评分:优(见图3)。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#肘关节脱位#
43
#肘关节#
42
#骨重建#
29
#关节脱位#
29
^_^^_^^_^^_^
39
#陈旧性#
29
#脱位#
25