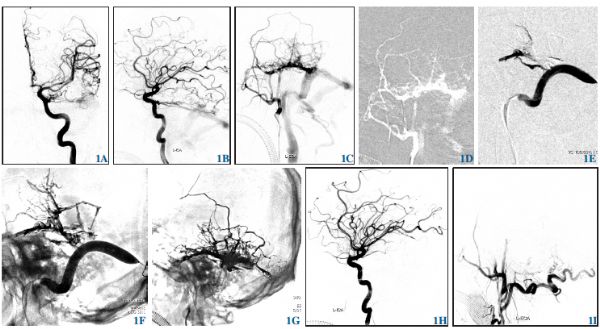
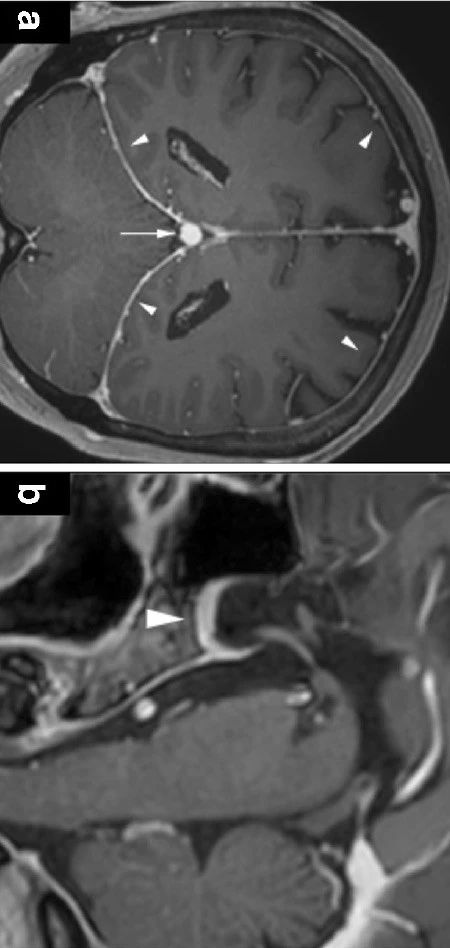
静脉窦球囊保护介入栓塞治疗侧窦区硬脑膜动静脉瘘
2019-12-27 苏伟 李伟 梁士凯 中国微侵袭神经外科杂志
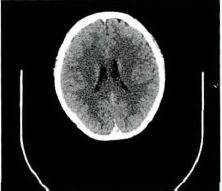
2016年7月-2017年12月北京清华长庚医院神经外科诊治侧窦区硬脑膜动静脉瘘(dural arteriovenous fistula,DAVF)病人12例,采取静脉窦内球囊保护技术来最大程度保留静脉窦通畅,分析栓塞治疗策略、球囊保护技术要点及并发症。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#静脉#
0
#球囊#
37
#动静脉瘘#
49
#静脉窦#
40
#硬脑膜#
45