颞下颌关节盘钙化病例报告
2019-12-11 宋娟 龙星 邓末宏 口腔疾病防治
颞下颌关节盘是颞下颌关节的重要组成结构之一,颞下颌关节紊乱病是口腔颌面外科临床常见的颞下颌关节疾病。颞下颌关节紊乱病常伴有关节盘的位置变化、形态改变,严重者出现关节盘的结构破坏。颞下颌关节盘钙化是一种少见的颞下颌关节盘病变,临床根据临床表现及影像学检查常难以与颞下颌关节髁突骨瘤、颞下颌关节滑膜软骨瘤并等鉴别,多依据手术中的发现及手术后病理检查方能确诊。
颞下颌关节盘是颞下颌关节的重要组成结构之一,颞下颌关节紊乱病是口腔颌面外科临床常见的颞下颌关节疾病。颞下颌关节紊乱病常伴有关节盘的位置变化、形态改变,严重者出现关节盘的结构破坏。颞下颌关节盘钙化是一种少见的颞下颌关节盘病变,临床根据临床表现及影像学检查常难以与颞下颌关节髁突骨瘤、颞下颌关节滑膜软骨瘤并等鉴别,多依据手术中的发现及手术后病理检查方能确诊。
武汉大学口腔医院近10年共收治颞下颌关节盘钙化病例2例,现对患者的临床表现及影像学特点进行分析,并对有关颞下颌关节盘钙化的文献报道进行回顾,以期对这一疾病的临床诊断提供帮助。
1.临床资料
病例1患者,女,57岁,2013年4月因左侧面部疼痛4个月入院。检查:开口度3.7 cm,左侧颞颌关节张口时可闻及杂音。螺旋CT提示左侧关节内钙化灶,多层螺旋CT(Multislice CT,MSCT)平扫左侧颞下颌关节窝及髁突骨质粗糙、硬化,髁突周围可见不规则斑片状钙化。患者术中发现病变的颞下颌关节盘出现大穿孔,关节上下腔联通。穿孔的关节盘残余部分分别向前后移位,残余的关节盘硬化,色泽及质地类似软骨,与周围的软组织无明显界限,钝性分离可游离出软骨块样组织。硬化的组织对应的髁突表面可出现压迫性吸收。病理学检查脱钙后的组织切片在显微镜下可见大量致密的成熟胶原纤维增生,胶原纤维中可见钙盐沉着;可见软骨细胞增生,大量细胞外基质形成并钙化(图1)。术后随访1年,疼痛消失,开口度4.0 cm。
图1 病例1影像学、病理学检查及手术切除标本。a:矢状面见髁突前、上、后可见高密度物质,髁突骨皮质可见被压迫吸收;b:横断面见髁突前高密度影像,髁突前内骨皮质压迫性吸收;c:手术标本病理学检查显示局部软骨细胞增生(A)、大量成熟胶原纤维增生(B)、细胞外基质钙化(C)HE×40;d:手术切除的软骨样组织块标本。
病例2,患者,女,37岁,2014年4月因后牙不能咬合1个月余入院。CBCT检查提示双侧颞下颌关节后内间隙增宽,局部可见点状钙化。螺旋CT平扫示双侧髁突粗糙不整,可见骨质增生,左侧明显,右侧关节间隙内可见不规则钙化。开口度4.0 cm,开口型正常,双侧关节外侧及后区压痛,双侧咬肌区压痛,右关节闭口末杂音。34~37、44~47牙开。术中见双侧关节盘穿孔,残余关节盘呈硬化的骨块(图2)。术后随访8个月,开口度4.2 cm,术后双侧后牙咬合恢复正常。
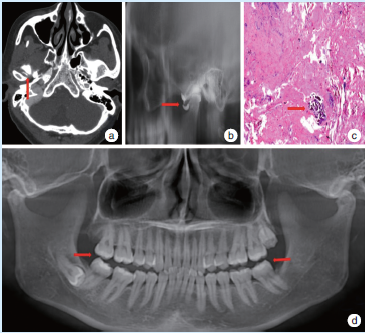
图2 病例2影像学及病理学检查。a:横断面见右侧髁突前钙化物;b:关节盘穿孔;c:组织内局部钙化HE×40;d:双侧后牙开。
2.讨论
2.1颞下颌关节盘钙化的病因
颞下颌关节盘钙化(calcification)在文献报道中有不同的名称,如关节盘内钙化组织(calcified tissue)、关节盘内肿瘤样钙质沉积(tumoral calcinosis)、钙化的关节盘(ossified articular disk)等。Marchetti等研究发现,钙化区由致密的矿化组织组成编织骨样的结构,内有不规则的细胞间隙,钙化区周围为富含细胞的矿化组织及各种排列的胶原。能量色散光谱分析,钙化区含有大量的Ca元素和P元素,X线衍射分析钙化的结晶为羟基磷灰石。
2.2颞下颌关节盘钙化的临床症状
文献报道颞下颌关节盘钙化患者住院的临床症状有开口受限、关节区疼痛,其他的症状可能有开口型偏向患侧、患侧后牙开及关节杂音,临床检查可能发现关节区肿胀及压痛。本文2例患者的症状表现除颞下颌关节疼痛、开口受限外,还可伴有双侧后牙开,文献未报道这一症状。
2.3颞下颌关节盘钙化的影像学检查
X检查是术前诊断颞下颌关节盘钙化的重要手段,曲面断层、CT、MRI检查均可发现颞下颌关节盘钙化。其影像学表现为髁突周围形态不一的高密度钙化灶,可伴有关节窝的骨质破坏及髁突骨质的退行性病变,也可表现为X线阻射性的关节盘样结构,同位素骨扫描可以显示局灶性活性升高。本文患者的影像学检查包括CT检查及关节造影,CT显示髁突周围高密度钙化灶,形态不一,这与文献报道相一致。在关节造影的检查中发现,关节盘钙化常伴有关节盘穿孔,这一影像学表现在手术过程中得到证实。
2.4颞下颌关节盘钙化的病理学检查
颞下颌关节盘钙化的病因目前尚不十分明确。Embree等通过手术在兔的颞下颌关节中制备关节盘穿孔模型,在手术后第8周即可在颞下颌关节盘穿孔的表面发现钙化。Embree等在这一研究中同时还证实颞下颌关节盘细胞在BMP2和骨生成介质存在的环境中能够矿化。有研究报道咀嚼产生的机械负荷也可以刺激局部细胞成骨。
综合上述报道,认为关节盘穿孔时的炎症介质可以引起骨祖细胞向穿孔区聚集,增殖分化成软骨并分泌出富含GAGs的细胞外基质,最终骨化。笔者在以往的临床关节盘穿孔的患者术后病理检查中发现,出现颞下颌关节盘穿孔的关节盘中常常伴有钙化形成,同时关节盘穿孔患者多数没有明显的颞下颌关节损伤病史,对此笔者认为,关节盘钙化的发生可能与咀嚼导致颞下颌关节盘受到的异常机械负荷有关。
2.5颞下颌关节盘钙化的鉴别诊断
临床上关节盘钙化需与髁突骨软骨瘤、滑膜软骨瘤病相鉴别。钙化的关节盘影像学表现为关节腔内游离的高密度影,与髁突骨皮质不相连续,形状多为不规则团块,数量为2~3个。髁突骨软骨瘤则表现为正常的髁突外形发生改变,表现为髁突上端或前斜面增生,与正常的髁突骨质相连的高密度影,临床可出现面部偏斜。颞下颌关节滑膜软骨瘤病的X线影像表现不一。成熟钙化的软骨瘤表现为关节腔内多个卵圆形的高密度游离影,一般不伴有关节盘穿孔,瘤体一般体积较小,数量可多达数十个。未骨化的软骨瘤则可在颞下颌关节造影检查中发现多个圆形或卵圆形的造影剂充盈缺损,关节镜检查可见到关节腔内游离体。
2.6颞下颌关节盘钙化的治疗
颞下颌关节盘钙化是一种良性病变,患者主要因颞下颌关节病区疼痛就诊。本课题组在手术中发现硬化的关节盘伴有关节盘穿孔,因穿孔过大残余的关节盘组织少而难以修补,故而本文2例患者均采用关节盘切除术。为了促进术后开口度恢复,术后第三天即鼓励患者开始开口锻炼。早期进软食为主,逐渐向普通饮食过渡。本文2例患者术后随访,关节区疼痛消失,术后开口度恢复正常,均未发现明显的咀嚼功能受限。患者未诉术后出现其他的并发症,据此认为,对于硬化的颞下颌关节盘可以单纯采用手术切除。
原始出处:
宋娟,龙星,邓末宏.颞下颌关节盘钙化病例报告暨文献回顾[J].口腔疾病防治,2018(01):48-51.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#颌关节盘#
43
#钙化病#
47
#下颌#
51
#颞下#
45
#颞下颌#
49
#病例报告#
37