EAU18 ︱魏强教授:人工智能在泌尿系肿瘤诊疗中的应用进展
2018-03-25 魏强 肿瘤瞭望
本届EAU大会首日,四川大学华西医院泌尿外科魏强教授团队的“利用机器学习模型预测及改善前列腺癌根治术后患者控尿功能”成果发言受到了与会学者高度关注。由于根治手术技术的日臻完善以及局限性前列腺癌具有较好的生存预后,患者术后的功能学结局(尿控、尿垫使用情况)及生活质量受到更多的关注。然而传统回归模型只能针对全人群绘制出统一的预测方程,很难满足精准医学及人民生活水平快速提升背景下医生临床决策及患者追
随着人工智能技术日趋成熟,其在医疗领域的应用正逐渐为疾病的诊疗带来技术上的革新。我们欣喜地看到,在本次欧洲泌尿外科年会(EAU)上诸多研究正在尝试将人工智能应用于泌尿系肿瘤的诊断。可以预见在不久的将来,这些技术的成熟与推广,将造福泌尿系肿瘤患者,同时也将使泌尿外科医生在诊断疾病时更加充满信心!
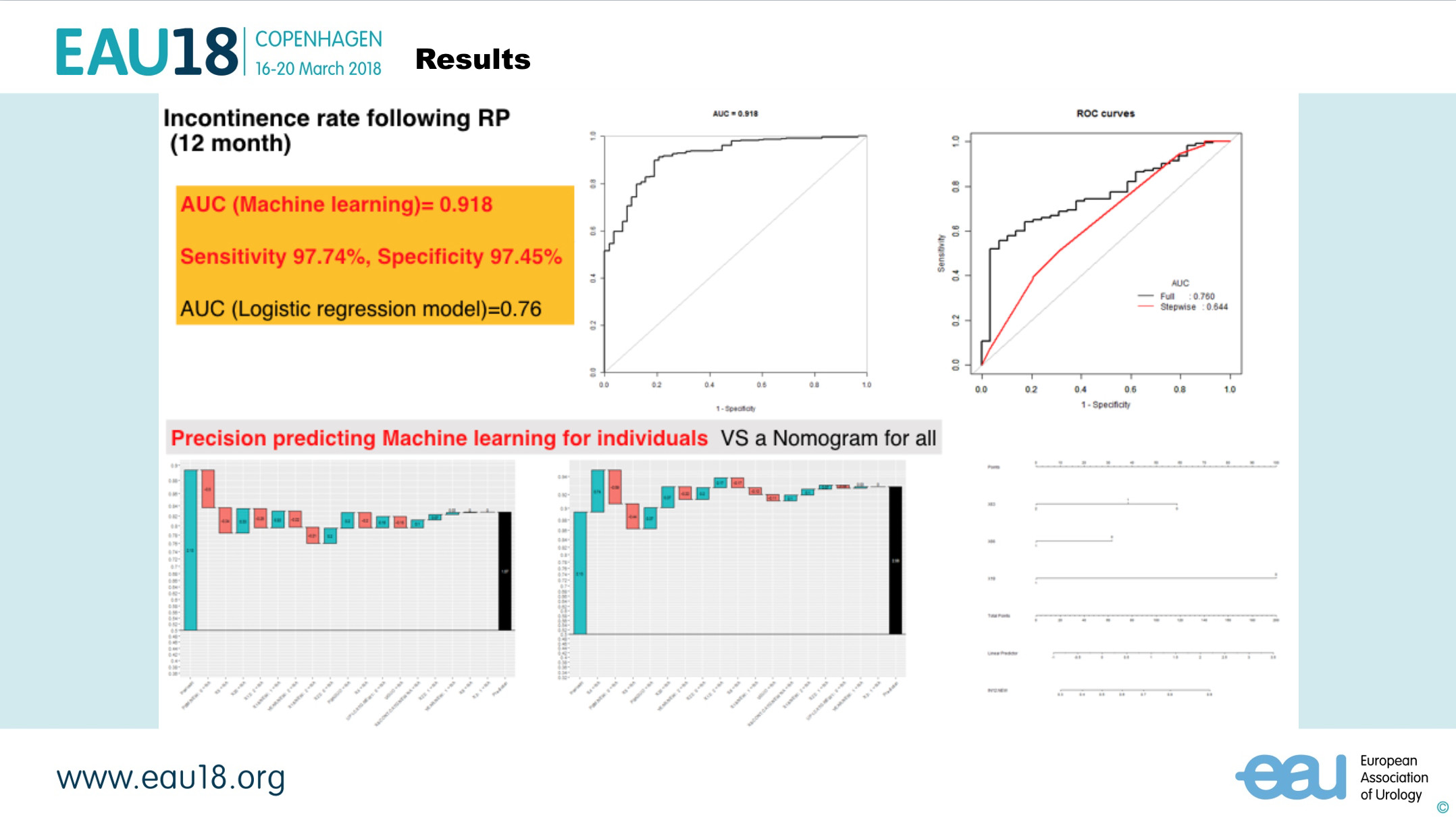
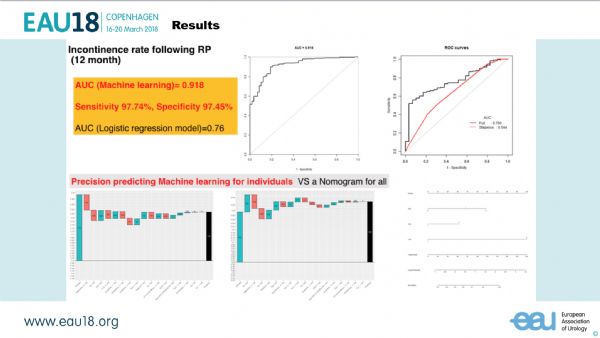
本届EAU大会首日,四川大学华西医院泌尿外科魏强教授团队的“利用机器学习模型预测及改善前列腺癌根治术后患者控尿功能”成果发言受到了与会学者高度关注。由于根治手术技术的日臻完善以及局限性前列腺癌具有较好的生存预后,患者术后的功能学结局(尿控、尿垫使用情况)及生活质量受到更多的关注。然而传统回归模型只能针对全人群绘制出统一的预测方程,很难满足精准医学及人民生活水平快速提升背景下医生临床决策及患者追求高质量生活的需要。
魏教授团队以中国多中心局限性前列腺癌队列大数据为基础,通过机器学习算法为每一位患者设计出“个性化”的尿控功能预测模型。该模型不仅可以为每一位患者做个体化预测(AUC=0.918/0.959), 亦可以使医生一目了然的了解到那些因素起主要作用,如果是可以干预的因素,在预测的同时给出下一步精准治疗的方案。
同时,来自南京鼓楼医院的张成伟医生向大家展示的利用人工智能诊断病理切片中前列腺癌癌灶的技术引人注目。该团队利用283名患者的918张组织病理学整体切片,依据病理医生的Gleason Score判定结果,利用深度机器学习大量的切片,最后对10名患者的10张切片进行验证,机器算法识别与病理学家的识别相似率高达99.38%。日后该技术的成熟与推广,将为前列腺癌穿刺或根治标本的精准分级带来颠覆性的技术革新与诊断效率的极大提高。
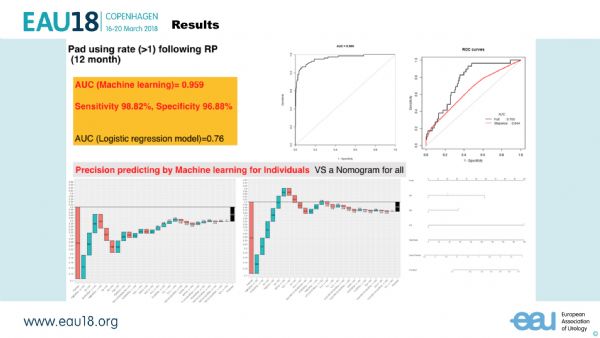
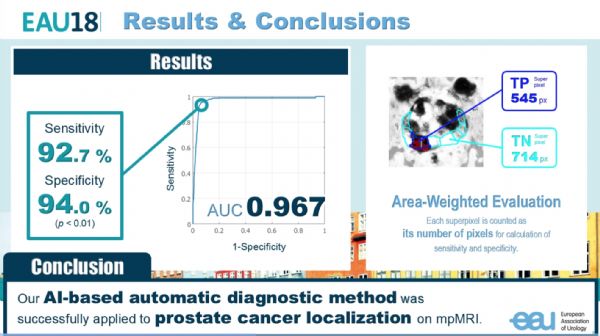
除了病理切片的精确诊断,如何利用人工智能填补影像科医生的缺口,利用现有的影像学手段,尽可能多地为泌尿科医生提供更多、更准确的信息,同样值得关注。本次大会上,来自日本国家先进工业科学和技术研究所的大石悠一郎纳入15名在2008-2017年间接受前列腺癌根治切除的患者,利用根治手术后病理切片勾画出肿瘤范围,然后将MRI的T2W1、ADC、DWI序列与根治标本的肿瘤范围进行精细到每一个像素点的一一对应,利用机器学习,敏感度和特异度分别达到了92.7%和94.0%,得到近乎完美的接收者操作特征曲线,使用AI自动诊断为MRI精确定位癌灶提供了可能性。
同样来自日本国家先进工业科学和技术研究所与筑波大学合作的另一项研究,则通过人工智能在膀胱镜下诊断非肌层浸润性膀胱癌。利该研究利用深度卷积神经网络,让机器通过阅读143张膀胱癌病灶的膀胱镜下图像(病理诊断确诊为膀胱癌),与107张正常膀胱组织图像,最终通过34张膀胱癌病灶镜下图像与28张正常组织图像进行检验,敏感度和特异度分别达到了93.1%和95.5%,该研究成果将来可以规避因为行镜检医生的观察偏倚造成的膀胱癌漏诊、误诊。
将人工智能用于泌尿系肿瘤的治疗,仍在研究和尝试的阶段。但是随着机器学习技术的不断优化与发展,在不久的将来,CT、MRI、病理组织学标本都将在人工智能的辅助下,为泌尿外科的医生和患者提供更多更准确的信息,进一步实现精准医疗!
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#泌尿系肿瘤#
39
#EAU#
0
#应用进展#
38
学习学习
80
学习了.谢谢!
71
#泌尿系#
20