NEJM:免疫治疗在晚期三阴乳腺癌III期临床试验中成功!中位总生存期提高61.3%
2018-10-23 奇点网 奇点网
《新英格兰医学杂志》便再次传来捷报。PD-L1抑制剂首次在晚期三阴乳腺癌临床Ⅲ期试验中取得重大胜利!该试验是由伦敦玛丽女王大学Peter Schmid教授领导的团队完成的。他们将免疫检查点抑制剂Atezolizumab与化疗药物白蛋白结合型紫杉醇(nab-paclitaxel)联用,与单独使用白蛋白结合型紫杉醇相比,PD-L1阳性的晚期三阴乳腺癌患者中位总生存期提升了近10个月,达到25个月,
《新英格兰医学杂志》发表最新的研究,PD-L1抑制剂首次在晚期三阴乳腺癌临床Ⅲ期试验中取得重大胜利!
该试验是由伦敦玛丽女王大学Peter Schmid教授领导的团队完成的。他们将免疫检查点抑制剂Atezolizumab与化疗药物白蛋白结合型紫杉醇(nab-paclitaxel)联用,与单独使用白蛋白结合型紫杉醇相比,PD-L1阳性的晚期三阴乳腺癌患者中位总生存期提升了近10个月,达到25个月,效果超乎预期[1]!
《纽约时报》评论道,这个结果意义重大,可能促使FDA批准将免疫疗法用于对三阴乳腺癌的治疗,并有望改变现在晚期三阴乳腺癌的临床治疗标准,为更多的癌症患者带来生的希望[2]。
免疫疗法已经在多种癌症的治疗中取得成功,包括肺癌,黑色素瘤等。但是在乳腺癌中却一直没有进展。
在很多其他癌症中,通常会存在很多突变“热点”,这些基因异常使得免疫系统能够将其识别并加以攻击,这是免疫治疗的基础。
但是乳腺癌细胞却相对较“冷”,拥有的突变更少,使得免疫系统难以识破其“入侵者”的身份,无法发动攻击。研究人员表示,这恐怕就是先前免疫检查点抑制剂在乳腺癌中不尽如人意的原因。
所以这次试验,科学家们给免疫检查点抑制剂请来了帮手——紫杉醇,一种天然的化疗药物。

紫杉醇提取自红豆杉,是一种天然的抗肿瘤物质
这里,研究者用到的是白蛋白结合型紫杉醇。白蛋白结合型紫杉醇实际上是现在治疗三阴乳腺癌的一线药物。三阴乳腺癌是乳腺癌里相对严重的类型,患者用白蛋白结合型紫杉醇进行治疗后,总生存期也不到18个月[3]。
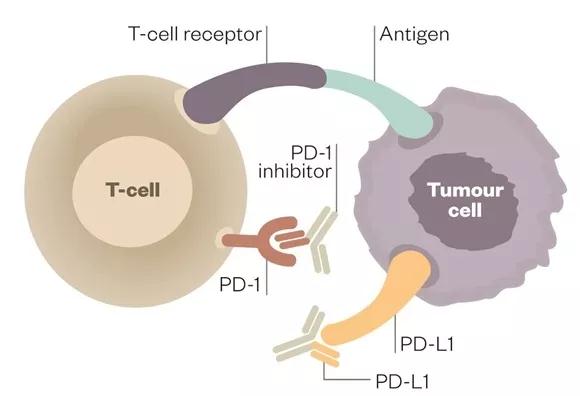
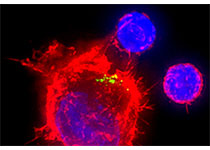
科学家发现在三阴乳腺癌肿瘤细胞会表达PD-L1,来压制浸润到肿瘤组织中的免疫细胞,并且这些PD-L1会集中在免疫细胞处。这表明免疫检查点抑制剂可能会在三阴乳腺癌中起作用!
于是,研究者们决定用一种PD-L1抑制剂——Atezolizumab,来试验免疫疗法治疗三阴乳腺癌的效果。
但是还有一个问题,就是我们上面提到的,免疫细胞难以识别乳腺癌细胞。怎么解决呢?白蛋白结合型紫杉醇!
白蛋白结合型紫杉醇可以增强肿瘤抗原的释放,提高免疫检查点抑制的抗肿瘤反应。此外,白蛋白结合型紫杉醇还能激活Toll样受体的活性,并增强树突细胞的活性[4]。白蛋白结合型紫杉醇可以使肿瘤细胞在免疫细胞面前无法隐身,从而能够被制裁!
想到了这个办法后,研究者们马上就开始行动了。
他们先在一个临床Ⅰ期试验中证明了Atezolizumab和白蛋白结合型紫杉醇联用的安全性,并且发现Atezolizumab的抗肿瘤活性也并未消失[5]。
而这次,正是Atezolizumab和白蛋白结合型紫杉醇联用的一个临床Ⅲ期试验,以白蛋白结合型紫杉醇和安慰剂作为对照。两个主要疗效终点是患者的无进展生存期和总生存期。
本次试验共募集了902名志愿者,都患有转移性或者局部晚期无法切除的三阴乳腺癌。研究人员将志愿者随机分配到Atezolizumab与白蛋白结合型紫杉醇联用组或白蛋白结合型紫杉醇组,每组各451人。患者都取了肿瘤组织样本,并做了PD-L1表达检测。这些患者来自41个国家的246个地区,个人信息都被登记。
研究者在患者使用药物后,对他们进行了随访。
随访结果显示,Atezolizumab和白蛋白结合型紫杉醇联用组的患者中位无进展生存期和中位总生存期分别为7.2个月和21.3个月。而白蛋白结合型紫杉醇组的中位无进展生存期和中位总生存期分别为5.5个月和17.6个月。白蛋白结合型紫杉醇和Atezolizumab联用显示了一定的优势,但并不显著。
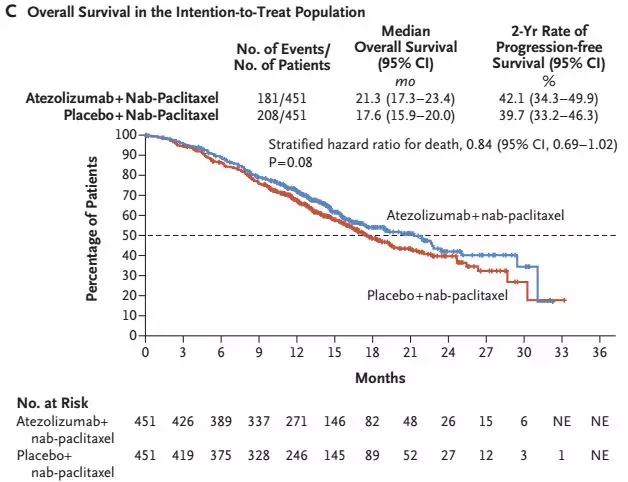
整体上看,联用组优势并不明显
我们知道,PD-L1抑制剂不是对所有的肿瘤患者都有效,需要肿瘤标志物进行疗效预测和指导,比如肿瘤突变负荷和PD-(L)1的表达等。
研究者们在募集志愿者时,根据PD-L1的表达情况,将志愿者分为PD-L1阳性和PD-L1阴性。其中PD-L1阳性的患者共有369人,185人被分配到了Atezolizumab和白蛋白结合型紫杉醇联用组,184人被分配到了白蛋白结合型紫杉醇组。
当将两组PD-L1阳性患者的数据进行比较时,他们发现了令人激动的结果!
在PD-L1阳性患者中,只用白蛋白结合型紫杉醇进行治疗的患者,中位无进展生存期和中位总生存期分别只有5.0个月和15.5个月:而用Atezolizumab和白蛋白结合型紫杉醇联合治疗的患者,中位无进展生存期和中位总生存期分别达到了7.5个月和25个月,联合治疗的优势非常明显!
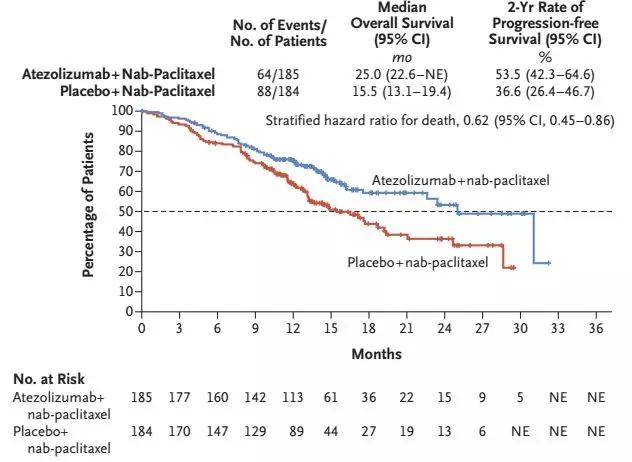
至此,我们可以说PD-L1抑制剂疗法在白蛋白结合型紫杉醇的帮助下,首次在三阴乳腺癌中取得成功,大幅延长了患者的生存时间!
此外,可喜的是,在这902名志愿者中,PD-L1阳性患者的比例高达41%。这表明超过四成的三阴乳腺癌患者都可能在免疫治疗中获益,相比其他很多肿瘤,优势非常明显!
作为本试验的参与者,Ramos女士患有晚期三阴乳腺癌。她被随机分配到了Atezolizumab和白蛋白结合型紫杉醇联用组。在治疗开始几个月后,肿瘤便开始萎缩,并且在距今九个月前一次CT扫描中,她的体内并没有发现肿瘤的信号。目前,Ramos仍然在进行免疫治疗。
Ramos表示,希望所有与癌症抗争的女士都能得到这种药的治疗,以挽救自己的生命。
事实上,这一天应该不会等很久了,生产这种药物的公司已经向FDA提交了本试验的数据[2]。相信FDA很快会批准将该药用于三阴乳腺癌的治疗。
此前来自Keytruda的早期研究,是一项Ib期研究(KEYNOTE-012)的其中一个队列,该队列调查了Keytruda单药疗法(每2周注射一次,剂量10mg/kg)用于PD-L1表达呈阳性的晚期三阴乳腺癌(TNBC)的治疗。截止2014年11月10日,采用实体瘤缓解评价标准(RECIST)评价的Keytruda抗肿瘤活性数据如下:总缓解率(ORR)为18.5%(n=5/27),完全缓解率(CRR)为3.7%(n=1/27),部分缓解率(PRR)为14.8%(n=4/27),疾病稳定率25.9%(n=7/27),疾病进展率为44.4%(n=12/27),实现缓解的中位时间为18周(范围7-32),有33%的患者肿瘤缩小。在6个月时,无进展生存率为23.3%,中位缓解持续时间尚未达到。
参考文献:
[1]https://www.nejm.org/doi/full/10.1056/NEJMoa1809615
[2]https://www.nytimes.com/2018/10/20/health/breastcancerimmunotherapy.htmlrref=collection%2Fsectioncollection%2Fhealth
[3] Gobbini E, Ezzalfani M, Dieras V, et al. Time trends of overall survival among metastatic breast cancer patients in the real-life ESME cohort. Eur J Cancer 2018; 96:17-24.
[4]Emens LA, Middleton G. The interplay of immunotherapy and chemotherapy: harnessing potential synergies. Cancer Immunol Res 2015;3:436-43
[5] Adams S, Diamond JR, Hamilton E, et al. Atezolizumab plus nab-paclitaxel in the treatment of metastatic triple-negative breast cancer with 2-year survival follow-up: a phase 1b clinical trial. JAMA Oncol (in press)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#II期临床试验#
38
#I期临床#
49
#III#
42
#I期临床试验#
34
#生存期#
43
#总生存期#
33
#II期临床#
38
#III期临床试验#
28
#III期#
29
学习了
83