JAMA Cardiol:三级医院远程诊断支持可降低农村医院STEMI漏诊率
2022-06-05 MedSci原创 MedSci原创
三级医院予以诊断支持可降低农村医院STEMI的漏诊率,从而提高初次再灌注治疗率
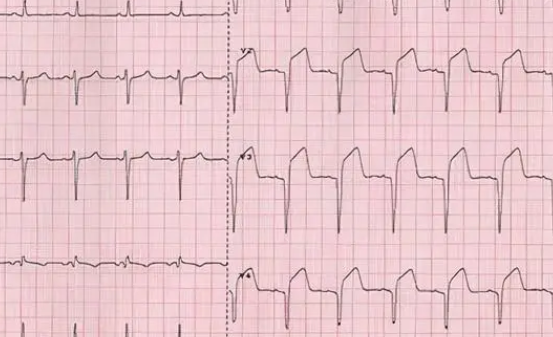
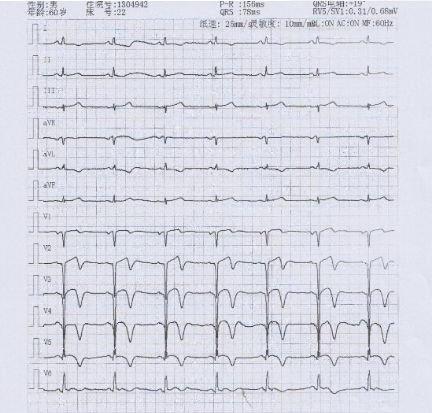
农村地区ST段抬高型心肌梗死 (STEMI) 的治疗包括溶栓,然后转移到具备经皮冠状动脉介入治疗能力的医院。第一步是通过心电图 (ECG) 进行诊断的,但约三分之一的STEMI会漏诊,因此未能得到及时治疗。
本研究旨在探究如何减少STEMI的漏诊。
这是一项在澳大利亚29个农村医院急诊科 (ED) 开展的整群随机临床试验,这些医院没有急诊医学专家。这29家医院被随机分成常规医疗组或自动触发三级转诊医院诊断支持(MORACS)组。纳入表现出与急性冠状动脉综合征 (ACS) 相符症状的患者。对症状符合ACS的患者进行分类可触发向三级医院冠状动脉监护病房的自动通知。三级医院医生通过远程查看心电图和床旁肌钙蛋白结果,并致电农村医院的主治医生以协助诊断和开始治疗。主要终点是STEMI的漏诊率。
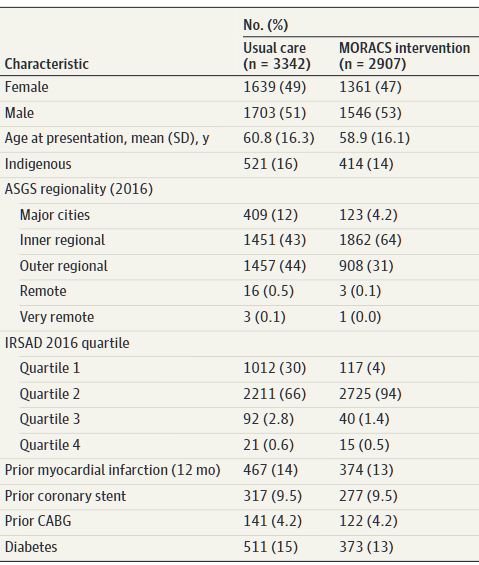
受试患者基线特征
共有6249位患者被纳入本研究分析(平均63.6岁,48%的女性)。在7474例疑似ACS的急诊就诊中,常规医疗医院和MORACS医院分别有77例(2.0%)和46例(1.3%)STEMI病例。常规医疗医院的77例STEMI中有27例(35%)被漏诊,而MORACS医院的46例中无一例漏诊(0%,p<0.01)。
不同分组患者的生存率
在符合条件的患者中,常规医疗组75位患者中的48位(64%)和MORACS医院的36位(100%)接受了初次再灌注治疗(p<0.001)。常规医疗医院和MORACS医院的12个月死亡率分别是10.3%和6.5%(相对风险 0.64)。与STEMI明确诊断的患者(2.0%)相比,STEMI漏诊患者的死亡率高达25.9%(相对风险 13.2,p=0.001)。总体上,有6位患者最终没有诊断STEMI,其中5位诊断为应激性心肌病,1位是心包炎。
综上,该研究提示,三级医院予以诊断支持可降低农村医院STEMI的漏诊率,从而提高初次再灌注治疗率。准确诊出STEMI可降低死亡率。
原始出处:
Dee F, Savage L, Leitch JW, et al. Management of Acute Coronary Syndromes in Patients in Rural Australia: The MORACS Randomized Clinical Trial. JAMA Cardiol. Published online May 25, 2022. doi:10.1001/jamacardio.2022.1188
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Cardiol#
41
#三级#
49
#农村#
39
#漏诊#
48
#STEM#
48
JAMA上文章都是顶级的,谢谢梅斯及时上新
35