Gynecol Obstet Invest:UAE治疗CSP后清宫时出血的危险因素
2015-05-16 MedSci MedSci原创
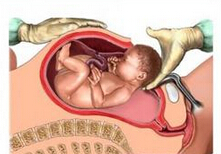
剖宫产术后子宫瘢痕处妊娠(CSP)是指孕卵、绒毛或胚胎着床于子宫既往剖宫产瘢痕处,是一种极罕见的异位妊娠,事实上是一种特殊的子宫肌层妊娠,是一种剖宫产远期并发症。近 几年随着剖宫产率的增高,此病发生率有明显升高趋势。子宫动脉栓塞术(UAE)是通过股动脉行Seldinger穿刺,将直径约3mm的导管在透视监视下送入子宫动脉,经造影证实导管已进入子宫动脉,而后释放栓塞剂栓塞子宫动脉,可以达到预防出血和
剖宫产术后子宫瘢痕处妊娠(CSP)是指孕卵、绒毛或胚胎着床于子宫既往剖宫产瘢痕处,是一种极罕见的异位妊娠,事实上是一种特殊的子宫肌层妊娠,是一种剖宫产远期并发症。近 几年随着剖宫产率的增高,此病发生率有明显升高趋势。
子宫动脉栓塞术(UAE)是通过股动脉行Seldinger穿刺,将直径约3mm的导管在透视监视下送入子宫动脉,经造影证实导管已进入子宫动脉,而后释放栓塞剂栓塞子宫动脉,可以达到预防出血和止血的作用。
对剖宫产术后子宫瘢痕处妊娠(CSP)进行贸然清宫,很容易出现大出血等并发症,而清宫前进行子宫动脉栓塞术(UAE)则为大出血等情况的发生提供了一定的保障,但是并不是说对切口妊娠患者行了子宫动脉栓塞就一定100%的不会出血。近期Du YJ等人专门就这一诊疗情况进行了病理对照试验,探究对剖宫产术后子宫瘢痕处妊娠(CSP)清宫前行子宫动脉栓塞术(UAE)后再清宫时的出血风险。
该研究共纳入了35名CSP患者,经过UAE治疗,在清宫过程中有出血情况,同时纳入140名清宫过程中没有出血的患者作为对照组。研究者收集了患者的孕周、妊娠物与膀胱距离以及阴道出血量等数据。
研究结果显示,经UAE治疗的患者中有6名进行了输血治疗,2名进行了子宫切除术,而对照组没有出现输血治疗或是子宫切除术等情况。研究者通过多变量分析发现,CSP组患者的出血与其孕周和妊娠物与膀胱距离有关。相比于对照组,CSP组患者孕周对出血的影响OR值为1.579 (95% CI 1.291-1.933);妊娠物与膀胱距离对出血的影响OR值为0.208 (95% CI 0.082-0.531)。
研究结果表明,对行了子宫动脉栓塞术(UAE)的剖宫产术后子宫瘢痕处妊娠(CSP)孕妇行清宫术,其孕龄越大,出血风险越大;而妊娠物距离膀胱>0.2 cm则其出血风险小。
原始出处:
Du YJ, Zhang XH, Wang LQ. Risk Factors for Haemorrhage during Suction Curettage after Uterine Artery Embolization for Treating Caesarean Scar Pregnancy: A Case-Control Study. Gynecol Obstet Invest. 2015 .
本文系Medsci原创编译整理!转载需要先获得授权,并附原文链接。谢谢!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#EST#
22
#NEC#
29
#TET#
25
#CSP#
49