NEJM:口哨音咳嗽-病例报道
2018-08-09 xing.T MedSci原创
虽然无法明确识别异物,但是在呼气末X射线照片中见空气滞留可以表明在支气管中存在吸入的异物,因为空气可以进入异物周围的支气管但不能排出。
患者为一名4岁的男孩,因持续咳嗽2天,间歇性口哨音而被送往耳鼻咽喉科门诊就诊。该患者没有上呼吸道病毒感染的病史或症状,并且感觉良好。他的父母报告说他在咳嗽开始前一直在吹口哨。
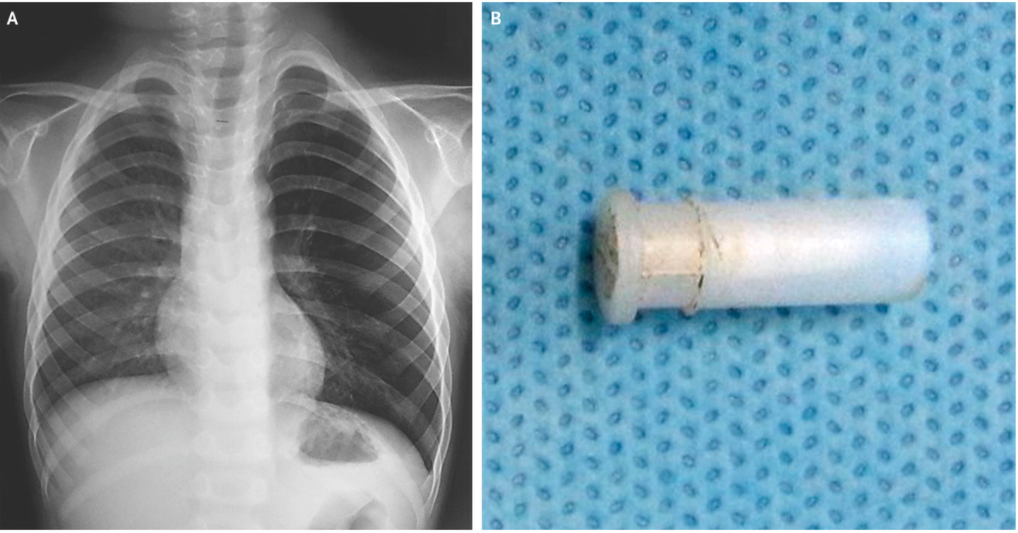
体格检查发现左侧中下肺呼气喘鸣,其余部分并不显著。胸部射线拍照显示左肺过度充气(如图A所示)。
虽然无法明确识别异物,但是在呼气末X射线照片中见空气滞留可以表明在支气管中存在吸入的异物,因为空气可以进入异物周围的支气管但不能排出。
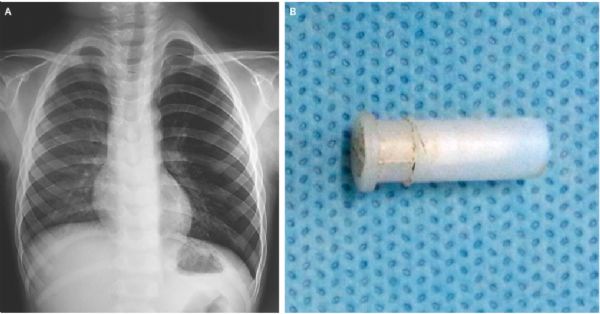
考虑到异物留在肺部的可能性,医务人员进行了硬性支气管镜检查,取出了阻碍左段支气管的玩具口哨(如图B所示)。在取出异物后的第二天进行重复胸片显示左肺过度充气消退。这名儿童在一年的随访中表现良好。
原始出处:
Suresh C. Sharma,et al. Whistling Cough.N Engl J Med 2018; https://www.nejm.org/doi/full/10.1056/NEJMicm1716704
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






学习了
54
学习了,谢谢分享
55
口哨音咳嗽提示支气管异物可能,学习了。
53
学习了
55