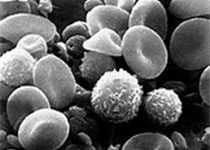
Blood:针对突变型RUNX1 AML细胞的靶向疗法
2019-04-27 MedSci MedSci原创
RUNX1转录因子可调节正常的和恶性的造血作用。体细胞或生殖细胞RUNX1突变(mt)与AML患者预后不良相关。敲除或抑制RUNX1可诱导更多的表达突变型RUNX1的AML细胞凋亡,提高表达突变型RUNX1的AML细胞的移植鼠的存活率。通过CRISPR/Case9介导敲除RUNX1增强子(eR1)或shRNA敲低BET蛋白BRD4抑制RUNX1的表达,可抑制突变型RUNX1 AML细胞的生长、诱导
用BET蛋白抑制剂(BETi)或降解剂(BET-PROTAC)抑制RUNX1及其靶点,可诱导细胞凋亡并提高突变型RUNX1 AML移植小鼠的存活率。LINCS1000-CMap数据库通过分析RUNX1敲除后的mRNA发现了一种新的表达模拟剂(EMs),可抑制RUNX1的表达,并可针对突变型RUNX1 AML细胞发挥作用。
EMs 华蟾蜍精、茴香霉素和秋水仙碱均可诱导AML患者来源的表达突变型RUNX1的造血祖细胞(HPCs)死亡,而且死亡率远高于来源于家族性血小板病(FPD)患者的HPCs或正常的未转化的HPCs。
本研究强调了针对表达突变型RUNX1的AML细胞的新型治疗药物。
Christopher P Mill, et al.RUNX1 targeted therapy for AML expressing somatic or germline mutation in RUNX1. Blood 2019 :blood.2018893982; doi: https://doi.org/10.1182/blood.2018893982
本文系梅斯医学(MedSci)原创编译,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#突变型#
36
#靶向疗法#
39
#RUNX1#
36
谢谢了,学习
82
学习学习学习学习
74