Chest:肺动脉高压患者管理中的药物相互作用
2022-07-19 刘少飞 MedSci原创
近年来,由于药物治疗选择的增加和伴随疾病数量增加的患者生存期延长,肺动脉高压 (PAH) 的管理变得更加复杂。因此,PAH 靶向药物和可能用于治疗合并症的药物之间存在更多的药物相互作用机会。
在20世纪80年代,在肺动脉高压(PAH)靶向医疗疗法出现之前,PAH(当时被称为原发性肺动脉高压)的长期预后很糟糕,一年的生存率只有68%,五年的生存率也仅34%。当时,PAH是一种年轻(平均年龄36岁)女性的疾病(女性与男性的比例为1.7:1),很少有合并症。在过去的25年里,PAH已经从一个没有具体治疗方法和令人沮丧的预后的疾病发展到一个有三个主要治疗途径和明显改善预期寿命的疾病。在同时代的REVEAL注册中,PAH诊断的平均年龄增加到50.1岁,并且在PAH患者中出现了更多的合并疾病。今天,超过2/3的特发性PAH患者有严重的合并症,这使得这一患者群体的治疗比过去更加复杂。不仅病人变得更加复杂,而且PAH的医疗管理的选择也增加了。现在有14种FDA批准的治疗PAH的药物以多种方式组合使用。目前批准的PAH靶向疗法主要作用于三个主要途径。一氧化氮途径(包括磷酸二酯酶5型(PDE-5)抑制剂,他达拉非和西地那非,以及可溶性鸟苷酸环化酶(sGC)刺激剂,利奥古特),内皮素途径(波生坦。内皮素途径(波生坦、安布生坦和马西坦)和前列环素途径(包括各种配方的前列环素类似物、依前列腺素和曲前列腺素,以及一种IP受体激动剂selexipag)。鉴于PAH患者在合并症和疾病具体管理方面越来越复杂,PAH药物与其他药物或合并症的补充剂之间存在许多药物相互作用的机会。
细胞色素P450(CYP450)是一种在药物代谢中起基础作用的酶。具有CYP450活性的药物可能是特定CYP450酶途径的抑制剂、诱导剂和/或底物,可改变同时服用的药物的代谢。抑制剂是指减少CYP450酶途径的物质,可能导致由同一途径代谢的其他药物浓度增加,导致药物毒性。
诱导剂是指诱导CYP450的一个酶途径的物质,它可能增加同一途径的其他药物的代谢,导致药物浓度低于治疗水平和治疗失败。尽管已经发现了50多种CYP450的异构体,但其中六种(CYP3A4、CYP2D6、CYP1A2、CYP2C9和CYP2C19)可以代谢90%的药物,其中最主要的两种酶是CYP3A4和CYP2D6。
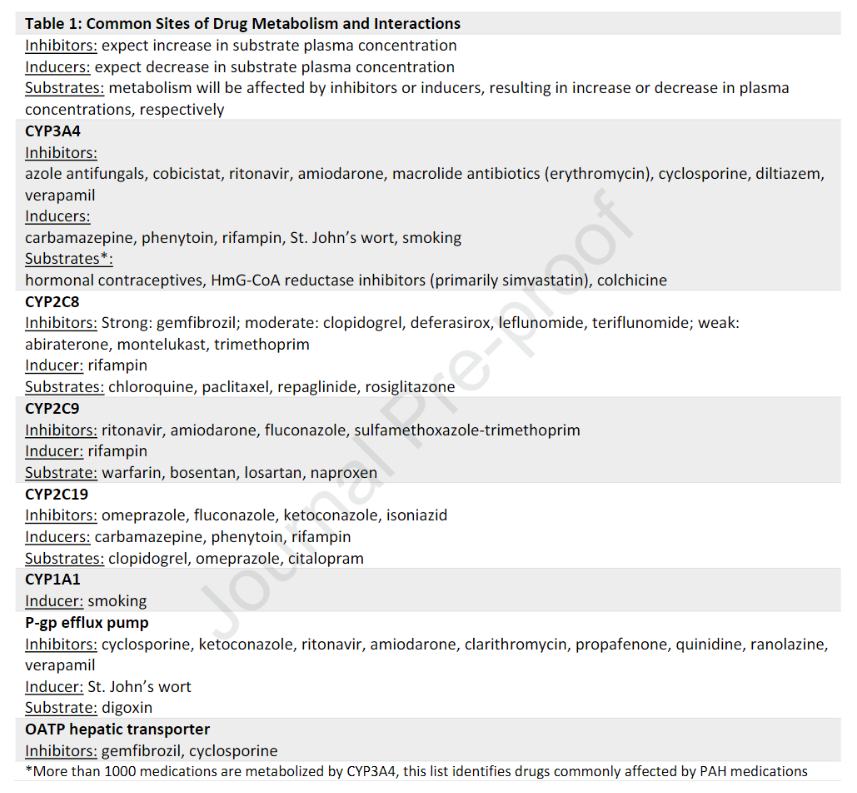
随着我们对CYP450代谢的认识不断加深,新药在上市前都要进行广泛的药物相互作用研究。然而,并不是所有的药物都经过了联合测试,有时药物的相互作用是根据已知的代谢途径来假设的。因此,药物间的相互作用可能包括放大已知的潜在不良反应。并非所有细胞色素P450介导的药物相互作用都具有临床意义,因此可能需要也可能不需要调整剂量。活性药物转运体、P-糖蛋白(P-gp)和人类有机阴离子转运多肽(OATPs)也在药物消除中发挥重要作用,并通过控制药物进入和离开细胞来影响一些药物的生物利用率。关于已知有CYP450、P-gp和OATP活性的常用药物。了解由CYP450酶代谢的药物、活性药物转运体以及最有效的 抑制和诱导药物的知识可以帮助最大限度地减少药物不良反应和相互作用或治疗失败的可能性。相互作用或治疗失败的可能性。
我们概述了细胞色素 P450 的药物代谢,并讨论了一氧化氮、内皮素和前列环素途径中 14 种 FDA 批准的 PAH 药物的重要药物-药物相互作用。在 NO 通路的靶标(西地那非、他达拉非和利奥西呱)中,与硝酸盐、蛋白酶抑制剂和其他磷酸二酯酶抑制剂的重要相互作用可导致严重的低血压。在内皮素途径中,波生坦通过 CYP3A4 抑制与更多的药物相互作用有关;macitentan 和 ambrisentan 的相互作用较少。虽然前列环素途径中的肠外治疗绕过了显着的肝脏代谢并避免了药物相互作用,但司来帕格和口服曲前列环素可能会与吉非罗齐和氯吡格雷等 CYP2C8 抑制剂发生相互作用,从而提高药物水平。最后,我们提供了一个框架来识别潜在的药物-药物相互作用并避免错误。这可以提高药物水平。最后,我们提供了一个框架来识别潜在的药物-药物相互作用并避免错误。这可以提高药物水平。最后,我们提供了一个框架来识别潜在的药物-药物相互作用并避免错误。
参考文献:
Wu S, Hoang HB, Yang J, Papamatheakis DG, Poch DS, Alotaibi M, Lombardi S, Rodriguez C, Kim NH, Fernandes TM. Drug-Drug Interactions in the Management of Patients with Pulmonary Arterial Hypertension. Chest. 2022 Jul 13:S0012-3692(22)01222-3. doi: 10.1016/j.chest.2022.06.042. Epub ahead of print. PMID: 35841932.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Chest#
44
#EST#
50
#肺动脉高压患者#
59
#动脉高压#
32
#相互作用#
40
学习
46
联合药物治疗肺动脉高压,有效但同时副作用也增加
40
#互作#
38
#患者管理#
43
#药物相互作用#
38