Infection: 接受抗生素治疗并不会改善新冠感染患者的全因死亡率和疾病进展
2022-03-27 MedSci原创 MedSci原创
众所周知,抗生素可以用来杀菌,通常被用来治疗炎症感染。那么,既然抗生素可以用来杀灭细菌,是否可以用来杀灭病毒呢?
我们已知在流感等呼吸道病毒感染中,细菌二重感染可导致更高的发病率和死亡率,需要及时诊断并开始抗生素治疗(ABT),有研究显示 COVID-19 感染患者的细菌合并感染和重复感染率低于10%,但全身性 ABT百分比超过 60%。目前没有足够的证据支持在 COVID-19 住院患者中需要广泛使用经验性 ABT,世界卫生组织 (WHO) 不建议对不复杂的 SARS-CoV-2 感染过程开始 ABT治疗,但建议对中度至重度疾病过程和临床怀疑细菌合并或重复感染进行ABT治疗。在全球 COVID-19 病例率居高不下的情况下,确定 ABT 的禁忌症和对治疗结果的影响,为医生提供决策策略至关重要。降钙素原 (PCT) 是一种经过验证的血清学标志物,可用于区分细菌性和非细菌性急性呼吸道感染。细菌感染会增强其从甲状腺外来源的产生和释放到循环中,低 PCT 表明细菌感染的可能性较低。本研究旨在探究ABT与 COVID-19 复杂阶段和低 PCT 值患者的全因死亡率和临床恶化的结果之间的关系。

研究人员分析了从2020年3月18日到2021年2月16日记录的 6457 例 SARS-CoV-2 感染病例。对于处于疾病复杂期且降钙素原 (PCT) ≤0.5 ng/ml 的成年患者,研究人员计算了任何抗生素治疗与全因死亡率/疾病进展到下一个更晚期疾病的相关性。同时考虑了混杂因素的性别、年龄和合并症的影响。
研究结果显示总共有三千六百二十七例符合分析患者被纳入本项研究。对于主要终点,研究人员发现抗生素治疗与较低的全因死亡率或进展到下一个更晚期阶段无关(p > 0.05)。对于次要终点,无论 PCT 水平如何,处于非复杂阶段 ( n = 1195) 的患者在接受抗生素治疗时,全因死亡率并没有降低,并且进入下一个更晚期(复杂)阶段的进展也没有减少(p > 0.05 )。PCT > 0.5 ng/ml 和抗生素治疗的复杂期患者 ( n = 286) 的全因死亡率显着增加 ( p = 0.029),但进展到关键阶段的概率没有显着差异(p > 0.05)。
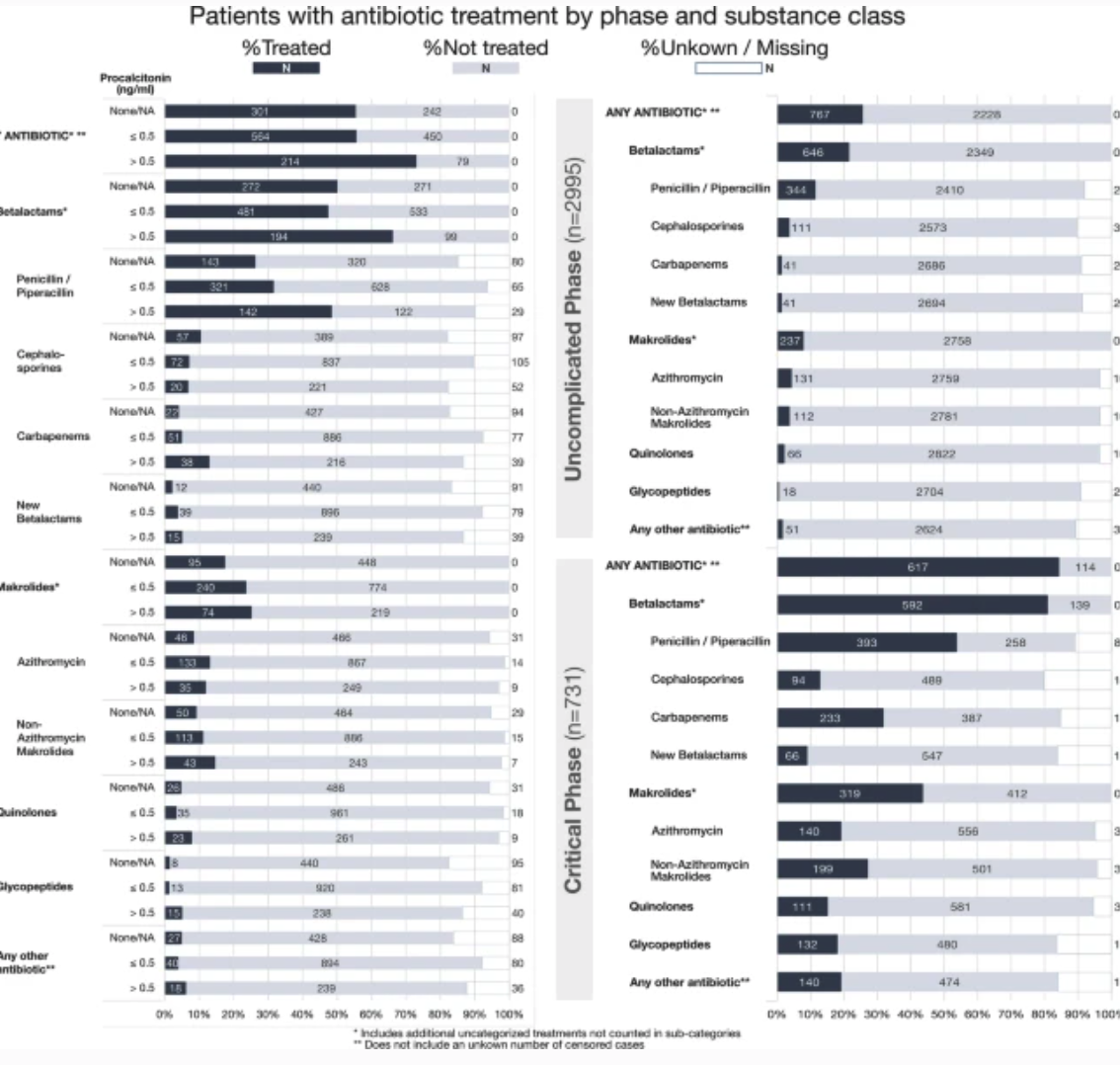
图:新冠肺炎患者的预后比较
本项研究证实在这个队列中,SARS-CoV-2 感染患者的抗生素与全因死亡率或疾病进展的积极影响无关,因此需要进一步改善 COVID-19 患者的合理抗生素使用。
Maximilian J. Schons. Et al. All-cause mortality and disease progression in SARS-CoV-2-infected patients with or without antibiotic therapy: an analysis of the LEOSS cohort. Infection.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#疾病进展#
40
#全因死亡率#
62
#抗生素治疗#
36
#Infection#
42
学习了
54