【病史临床】
患者,男,38岁,间断性咳嗽、咳痰,痰中带血丝半年,无发热、胸疼。
【影像图片】








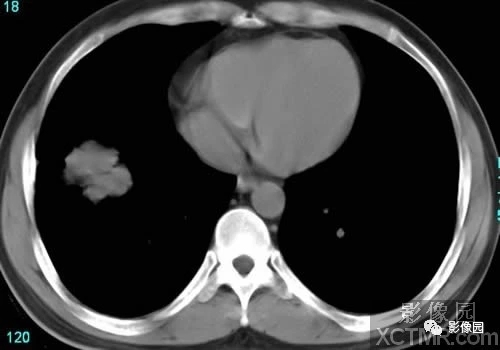



CT图像特点:
右肺下叶前基底段可见一软组织肿块影,大小36mmx39mm,密度均匀,CT值35HU,形态不规则、分叶状,边缘毛糙,并可见胸膜凹陷征,气管主支气管通畅,纵隔内未见明显肿大淋巴结影。余肺野内未见异常密度影。
影像:
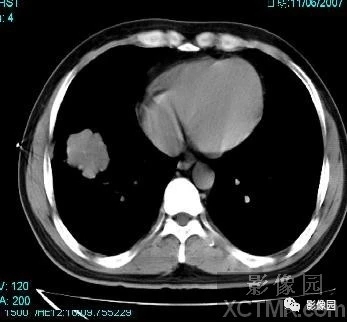
CT穿刺:
CT引导下行右肺下叶肿块穿刺活检术。
患者仰卧于CT检查台上,首先行胸部CT扫描确定病变位置。在局麻下行CT引导下肺部肿块穿刺活检术。常规消毒、铺巾、局麻。在CT引导下使肺活检针经右侧腋中线水平进入病变预定位置。在病变预定位置多点、多方向抽取小米样病变组织多块并涂片8张。术后穿刺点局部无出血,未出现气胸、胸腔出血等并发症。术中及术后患者生命体征稳定,未出现不适症状。
病理结果:小细胞癌。
点评:
CT检查对SCLC的诊断具有重要价值,同时, CT对肺癌的术前分期也具有重要作用。研究发现SCLC以长轴进展型最多见,周围肿块型相对较少 。长轴进展型因为其癌组织主要是在黏膜下生长,以向管外发展为主,侵袭力强,淋巴转移早,X线平片与CT扫描图像可见肺门与肺门旁的肿块或纺锤型阴影,同时伴有肺门、纵隔多发淋巴结的转移甚至融合。但是肺不张及阻塞性肺炎则相对少见,此特点与SCLC有明显的不同,根据CT影像提出疑诊SCLC者可达80% ,如能结合CT 导向经皮穿刺活检及纤维支气管镜检,可使诊断率达到90% 左右。不仅可以定性,还可以进行TNM分期,使SCLC患者选择治疗方案与判断预后不可或缺少临床资料。由于4级以下小支气管因其管壁薄,软骨成分少,因而周围肿块型SCLC 的癌组织易于穿破支气管壁向肺组织侵润发展。由于SCLC 生长速度快,所以在正常组织尚未出现免疫反应之前,癌肿即可以达到相当大的体积。术后切除标本的剖面观察与局部切片镜检,可见周围肺组织出现压迫性肺不张,呈现假“包膜” 现象。CT影像学资料可表现为边缘光滑的肿块,但未见渗出及增生反应。临近肺血管、支气管可以呈现挤压和推移的征象而酷似良性病变,所以当影像学资料疑诊SCLC时,必须进行短期随访和经皮穿刺活检及纤维支气管镜检加以确诊。由于SCLC病灶小,常规扫描不能清楚地显示病灶的内部细微结构和边缘征象,此时进行薄层扫描对病灶的显示有很大帮助。有学者研究认为在小肺癌的CT诊断中,如果有两个基本CT征象和一个以上次要CT征象便可确诊,其诊断准确率高达90%。周围型小细胞肺癌的基本X线征象,表现常不典型,多种多样。最常见的孤立性结节影,呈圆形或椭圆形,边缘不清,体层片可显示阴影边缘毛糙,堆集征,细小毛刺及分叶等。平片上的小片状浅淡影,在CT片上的征象为孤立结节影,较平片显示更多征象。其基本征象有分叶征、边缘毛刺征、血管集束征、空泡征和胸膜凹陷征,其各种征象均高于常规胸片。在周围型肺癌其他间接征象中,如蜂窝征、小空洞、病灶胸膜侧放射影,平片显示较差(平片出现率约20% ) 。在检查中出现率较高的有分叶征、毛刺征、胸膜凹陷征,对周围型小细胞肺癌的诊断有较高价值。但血管集束、小泡征也具有一定特征性 。
SCLC虽然有上述影像学特点,长轴进展性可以根据CT 表现提出疑诊,但是难以和淋巴瘤、转移癌、结核等病变相鉴别;而周围肿块型边缘光滑,酷似良性病变,更加难以确诊。而痰的细胞学检查阳性率低,纤维支气管镜检查虽然可以发现支气管黏膜增粗,纵行皱襞,血管怒张,软骨轮廓消失与管腔狭窄等改变。但缺乏息肉或菜花状的新生物,钳取的癌细胞易于受到挤压而变形,造成细胞学诊断上的一定困难。但是,SCLC的肺门旁肿块、肺野肿块和纵隔内转移肿大的淋巴结均可以通过CT导向经皮穿刺活检取材送细胞学与组织学检查,诊断的敏感性与准确性可以达到90%左右。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#CT病例#
61
#小细胞癌#
48
#右肺#
48
#细胞癌#
43
#影像诊断#
49
学习
65
学习了
78