J Hepatology: Toll样受体4是预防和治疗肝衰竭的治疗靶标
2020-02-22 不详 MedSci原创
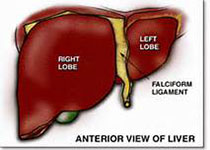
Toll样受体4(TLR4)在介导急性肝衰竭(ALF)和急性慢性肝衰竭(ACLF)的器官损伤中起重要作用。在这里,研究人员评估了抑制TLR4信号传导是否可以改善肝功能衰竭并作为一种潜在的治疗方法。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#J Hepatology#点击进入话题查看更多相关文章 或评论时插入话题加入讨论
81
#治疗靶标#
38
#肝衰#
0
#靶标#
29
#EPA#
38