导读:p53是一个拥有广泛而强大功能的抑癌基因,作为转录因子,p53激活或者抑制多种下游靶基因的转录来行使功能。这些靶基因的作用主要包括诱导细胞周期停滞、DNA修复、调节细胞代谢、细胞衰老、细胞凋亡,以及新近发现的诱导细胞发生铁死亡等。
8月17日,纪念斯隆-凯特琳癌症中心于《Nature》发表了一项研究“Ordered and deterministic cancer genome evolution after p53 loss”,这项研究发现在胰腺转化环境中 p53 失活后的肿瘤进化不是随机的,而是受制于引起Trp53突变肿瘤的基因组和生物学特点的确定性特征。
Doi: 10.1038/s41586-022-05082-5.
研究背景
01
TP53作为肿瘤抑制基因,其失活突变与肿瘤侵袭性及肿瘤治疗抵抗密切相关,目前对于p53的研究认为p53 与DNA 损伤诱导的细胞周期检查点有紧密联系,且其失活可导致基因组不稳定。后续研究表明,p53 在转录上协调一系列广泛的细胞命运程序,这些程序积极地限制了肿瘤的发生,而破坏这些程序对于肿瘤维持仍然至关重要。然而,由于标记p53 失活后的细胞较为困难,尚不能确定基因组不稳定性如何准确地表现和塑造TP53 突变谱系发生的转变。
研究过程
02
为进行散发性p53杂合性缺失的谱系追踪,研究人员选取致癌基因Kras G12D等位基因的条件激活和Trp53的单个条件失活等位基因驱动的小鼠胰腺癌模型(KPC模型),并对KRAS及p53突变进行荧光标记,进行小鼠胰腺癌中散发性 p53 失活后早期癌细胞的谱系追踪(图1)。
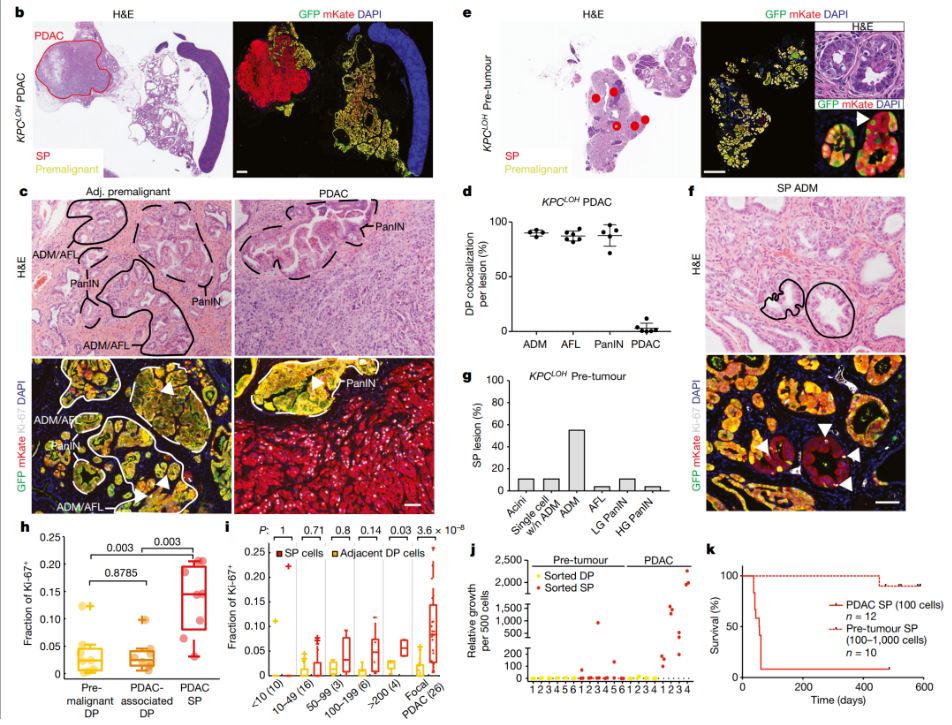
图1. 小鼠胰腺癌中散发性 p53 失活后早期癌细胞的谱系追踪
基于上述谱系追踪方法,研究人员在整个胰腺癌进展过程中对细胞进行了体内基因分型,并发现在 p53 失活后,靶向胰腺癌驱动因子的复发性和保守的拷贝数改变塑造了恶性基因组的进化,这意味着 p53 中的拷贝数进化改变了p53的 PDAC 结果失活并且不需要突变p53的功能增益效应。而这种独特而有序的基因组进化方式会导致组织由良性到恶性的改变(图2)。

图2. 独特而有序的基因组进化伴随着良性到恶性的转换
为进一步明确p53缺失后有序的基因组改变,研究人员对单细胞测序数据进行了进一步的分析,结果表明p53杂合性缺失后基因重排的选择是由确定性原则支配的,这种确定性原则揭示了胰腺癌进展过程中基因组进化的模式:先是p53的杂合缺失,然后是缺失的积累、多倍体的出现,然后是拷贝数突变累积(图3)。
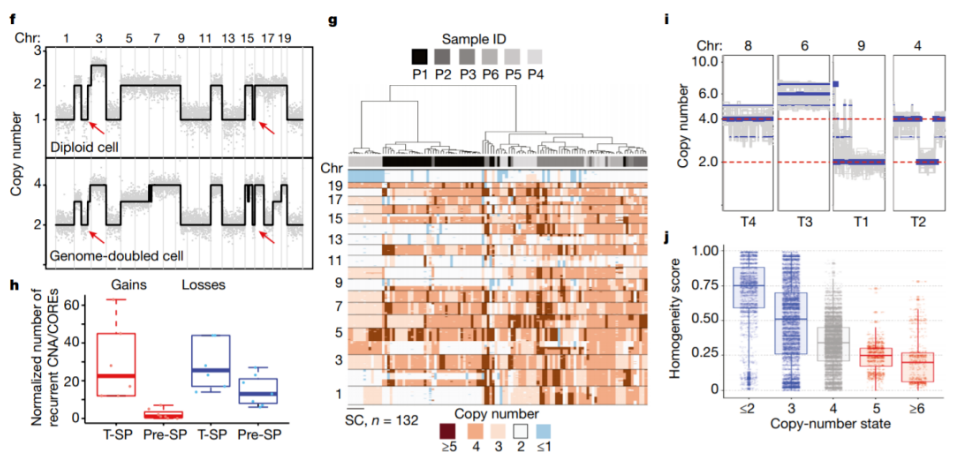
图3. 确定性原则决定p53杂合突变后基因组重排的选择
研究意义
03
这项研究表明,癌症的不同阶段的进展过程中伴随着由p53缺失到后续基因组重排的有序过。在肿瘤进展后期,药物治疗的效果就会显著下降,而在肿瘤早期靶向治疗能取得最佳的效果,因此,靶向肿瘤早期p53的缺失性突变可能会带来肿瘤治疗的新方式。
参考资料:
Baslan T, Morris JP 4th, Zhao Z, et al. Ordered and deterministic cancer genome evolution after p53 loss. Nature. 2022 Aug 17. doi: 10.1038/s41586-022-05082-5.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Nat#
0
#治疗格局#
43
#肿瘤治疗#
50
#p53#
48