Lancet Neurol:持续不断地提高CAS围手术期安全性
2019-05-31 杨中华 脑血管病及重症文献导读
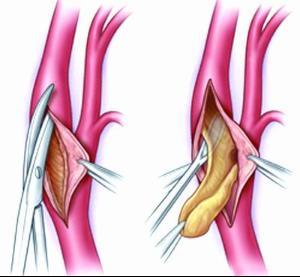
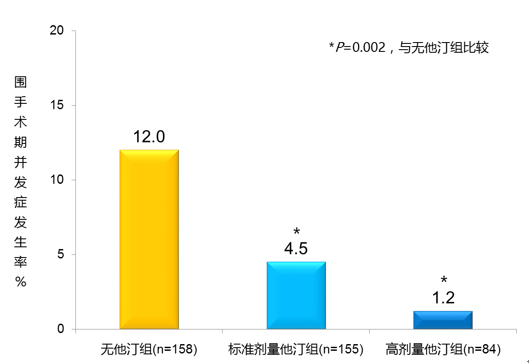
对于症状性颈动脉狭窄患者,一些研究发现颈动脉支架(CAS)的围手术期卒中或死亡风险高于颈动脉内膜剥脱术(CEA),但是两种技术的长期结局尚未被充分评价。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#手术期#
32
#Neurol#
24
#Lancet#
21
#Cas#
24