Lancet Oncology:局部晚期头颈肿瘤的放化疗:一项个体患者数据网状荟萃分析
2021-05-24 MedSci原创 MedSci原创
局部晚期头颈肿瘤的治疗进展使治愈率较前增加。对头颈肿瘤化疗(MACH-NC)的个体患者数据进行荟萃分析,结果表明,在放疗的基础上联合化疗可提高总生存率、无进展生存率和局部控制率,减少癌症死亡。
局部晚期头颈肿瘤的治疗进展使治愈率较前增加。对头颈肿瘤化疗(MACH-NC)的个体患者数据进行荟萃分析,结果表明,在放疗的基础上联合化疗可提高总生存率、无进展生存率和局部控制率,减少癌症死亡。随机对照试验和荟萃分析表明,联合放化疗或超分割放射治疗对局部晚期头颈肿瘤患者具有生存益处。然而,这些疗法的相对疗效尚不清楚。

本文根据个体患者的荟萃分析数据进行了频率学网状荟萃分析,这些荟萃分析评估了化疗(头颈部肿瘤化疗荟萃分析[MACH-NC])和分次放疗(头颈部肿瘤放疗荟萃分析[MARCH])。本研究纳入了1980年1月1日至2016年12月31日期间招募的非转移性头颈部鳞状细胞癌患者的随机对照试验。研究主要使用两步随机效应方法和对数秩检验,通过试验分层来比较治疗,总体生存率是主要终点。

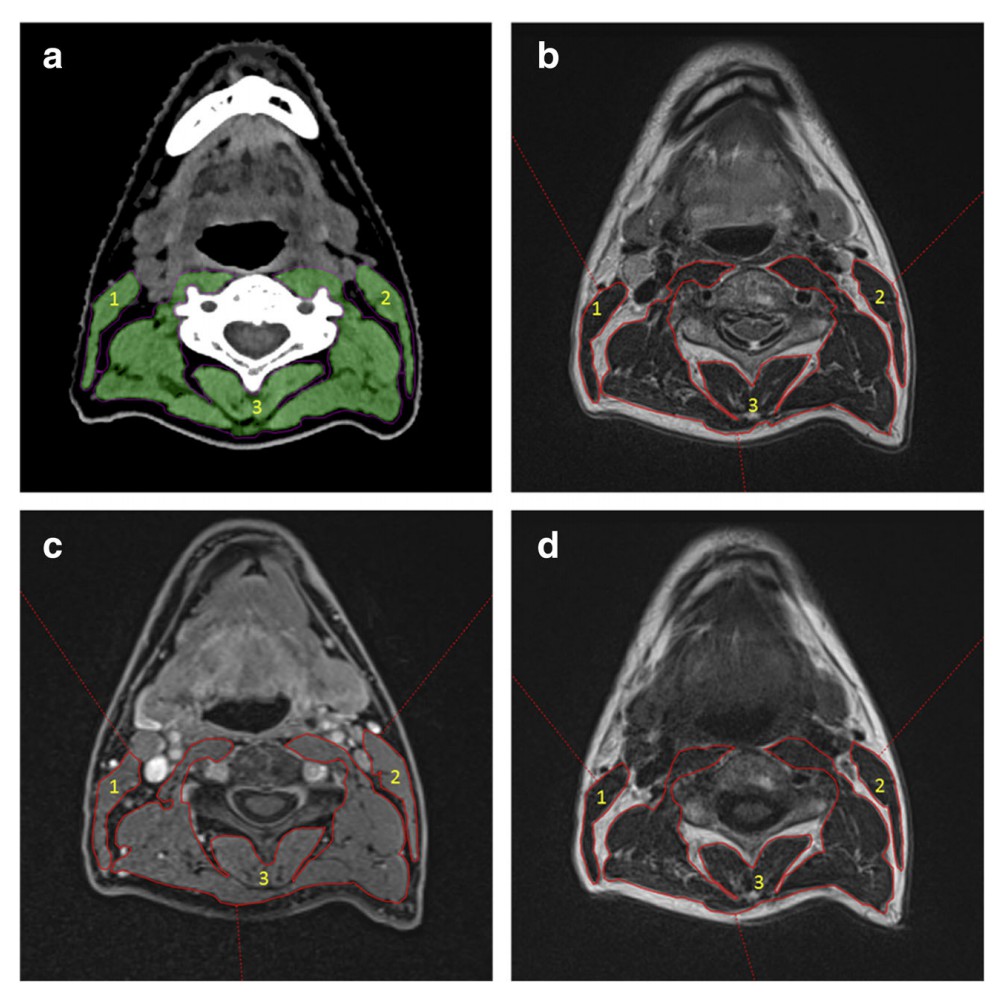
图1:总体生存率试验网络图
在1980年1月1日至2012年4月30日期间纳入患者的115项随机对照试验得出154项比较结果(28978名患者中有19253例死亡,20579例进展事件)。治疗分为16种模式,其中35种类型的直接比较是可用的。所有试验的平均随访时间为6.6年(IQR 5.0-9.4)。 超分割放疗联合化疗(HFCRT)是治疗总生存率的最佳方法(与局部治疗相比,P值97%;危险比0.63[95%CI 0.51-0.77])。与基于铂类化疗的同步放化疗(CLRTP)相比,HFCRT的总生存风险为0.82(95%CI 0.66-1.01)。HFCRT的优越性对敏感性分析是可靠的。
与CLRTP相比,其他三种治疗方式的总生存率P值更好,但HR没有显著改善(P值78%):紫杉烷、顺铂和氟尿嘧啶诱导化疗,随后局部治疗(ICTaxPF-LRT;89%)、加速同步放化疗(82%)和ICTaxPF后 CLRT(80%)。
综上所述,这种网状荟萃分析允许评估多种治疗方式并表明HFCRT优于其他治疗方法。
Petit, ClaireAdelstein, D.J. et al. Chemotherapy and radiotherapy in locally advanced head and neck cancer: an individual patient data network meta-analysis. The Lancet Oncology, Volume 22, Issue 5, 727 - 736
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Oncology#
40
#局部晚期#
39
#荟萃分析#
36
#Oncol#
39
#患者数据#
45
#荟萃#
31
#Lancet#
31
学习了,谢谢分享
65
#放化疗#
43
#局部#
30