先天性左心室-冠状静脉窦瘘一例
2018-06-09 聂谦 孔较瘦
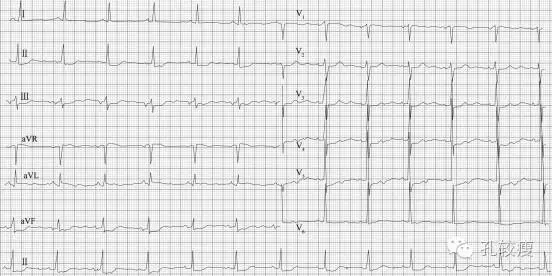
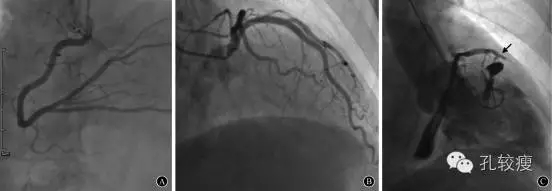
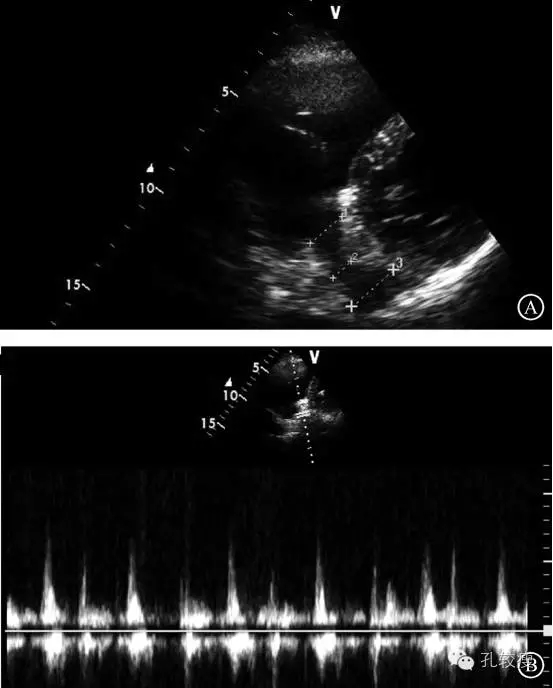
患者男性,78岁,因“反复胸闷、胸痛10年”于2015年11月20日入院。入院前10年,患者开始逐渐出现活动后胸闷、胸痛、无心悸,无咳嗽咳痰,无头晕黑矇,无反酸烧心等不适。患者在当地医院多次行心电图检查均提示“前壁心肌缺血”,给予硝酸酯类治疗后,患者自觉症状有所好转,但仍时有发作。入院前1周,患者胸痛症状再发,并伴有心悸,为求治疗患者转成都中医药大学附属医院就诊,入院查体提示心脏相对浊音界向右扩大
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#静脉#
45
#先天性#
39
#左心室#
42
#静脉窦#
50
好
66
不错的文章值得拥有哦
65