Cancer Discovery:余棣华团队发现,维生素E能够提高癌症患者生存率,通过激活树突状细胞,增强癌症免疫治疗效果
2022-04-19 王聪 生物世界
2022年4月14日,MD安德森癌症中心余棣华教授团队在 Cancer Discovery 期刊发表了题为:Vitamin E Enhances Cancer Immunotherapy by Rei
2022年4月14日,MD安德森癌症中心余棣华教授团队在 Cancer Discovery 期刊发表了题为:Vitamin E Enhances Cancer Immunotherapy by Reinvigorating Dendritic Cells via Targeting Checkpoint SHP1 的研究论文。
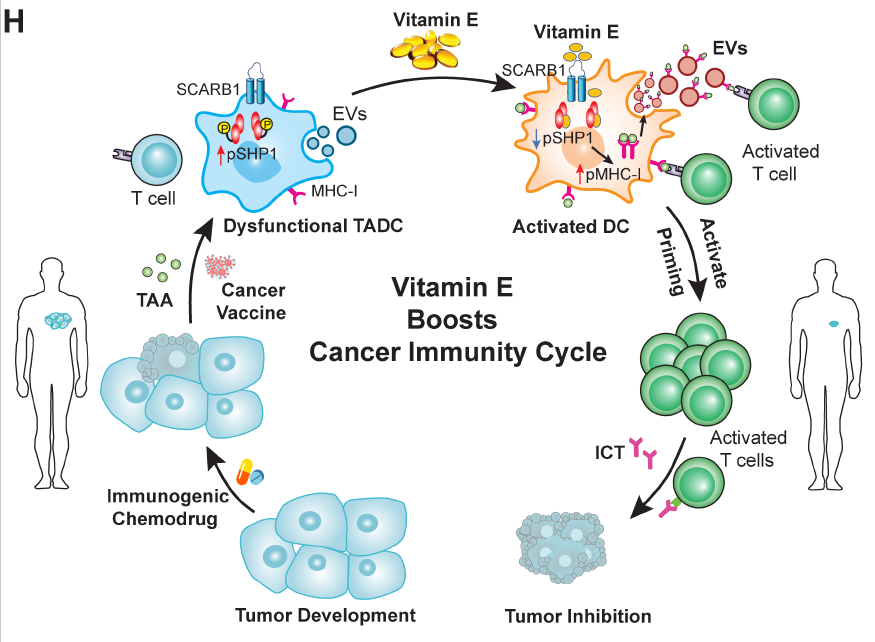
研究团队将临床记录的回顾性分析与实验室研究结合,发现维生素E直接结合并阻断树突状细胞中的免疫检查点蛋白 SHP1,从而激活树突状细胞活性,增强抗原呈递并启动 T 细胞抗肿瘤免疫反应。
该研究提出了改善癌症免疫治疗的新方法,包括与维生素E的联合治疗,或直接靶向抑制树突状细胞的 SHP1。

该研究的通讯作者、MD安德森癌症中心终身教授余棣华教授表示,这项研究拓宽了我们对可能影响免疫疗法反应的因素的理解。这项研究证明了维生素E通过抑制 SHP1 重新激活树突状细胞的抗原呈递,提示了我们维生素E处理或 SHP1 沉默的树突状细胞和树突状细胞来源的细胞外囊泡可以用来开发未来的癌症免疫疗法。

维生素E与免疫治疗反应的改善有关
免疫检查点抑制剂是近年来发展起来的一种癌症免疫疗法,被认为是改变了癌症治疗格局的重大突破。MD安德森癌症中心的 James Allison 也因为在免疫检查点疗法领域的贡献而获得了2018年的诺贝尔生理学或医学奖。
免疫检查点抑制剂可谓许多癌症患者提供持久的治疗反应,但并非所有癌症患者都能受益,因此,有必要了解患者产生不同反应背后的原因,从而改善更多患者的预后。
膳食补充剂被认为可以增强免疫力,但人们对膳食补充剂对免疫治疗活性的影响知之甚少。为了探索这种联系,余棣华团队对在MD安德森癌症中心接受免疫疗法治疗的癌症患者的临床数据进行了回顾性分析。
研究团队发现,相比那些不服用维生素E或多种维生素的 的接受 PD-1/PD-L1 免疫检查点抑制剂治疗的黑色素瘤患者,接受 PD-1/PD-L1 免疫检查点抑制剂治疗的同时服用维生素E的黑色素瘤患者的生存率更高。
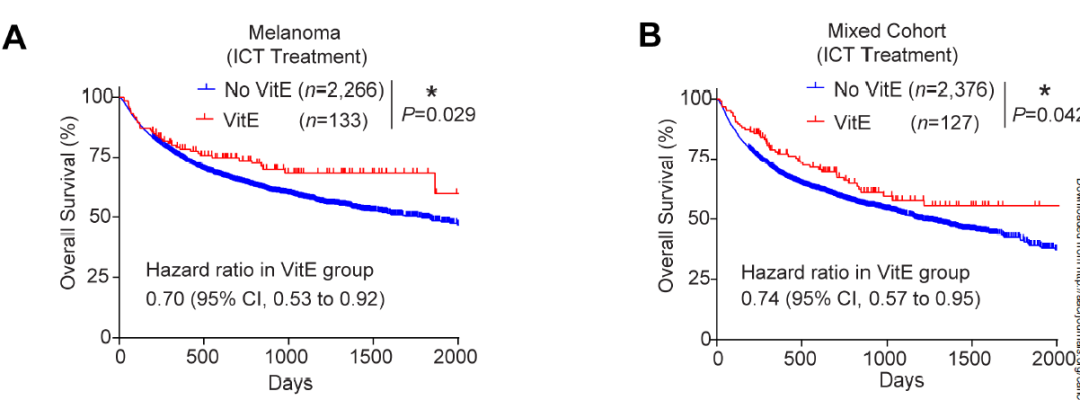
这一发现在乳腺癌、结肠癌和肾癌患者的独立混合队列中得到了验证。然而,在接受化疗的同时服用维生素E却没有获得相同的益处,这说明,维生素E的这种效果与化疗无关。
接下来,研究团队发现,维生素E增强了乳腺癌和黑色素瘤小鼠模型对免疫检查点抑制剂的反应。但具有低水平肿瘤浸润树突状细胞的小鼠没有从维生素E中获益,这说明维生素E的效果取决于肿瘤浸润树突状细胞。
破译维生素E对树突状细胞的影响
树突状细胞是一类特殊的免疫细胞,负责将将抗原呈递给 T 细胞,即发挥抗原呈递作用,这是抗肿瘤免疫反应的重要步骤。然而,由于肿瘤微环境中的抑制信号,肿瘤相关树突状细胞可能会变得功能失调,无法发挥抗原呈递作用。
研究团队发现,维生素E治疗会导致树突状细胞上的几种激活标志物上调。此外,与对照相比,用维生素E治疗的肿瘤的树突状细胞促进了更多的 T 细胞增殖,这表明维生素E增强了抗肿瘤免疫反应。
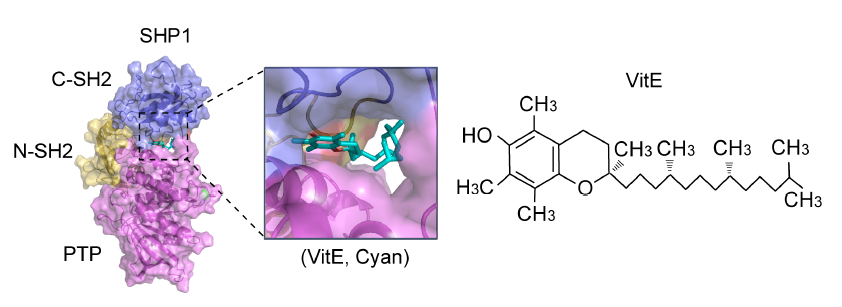
通过分子和结构研究,研究团队发现维生素E能够进入树突细胞并与其 SHP1 蛋白结合,SHP1 是调节树突细胞活性的免疫检查点蛋白,阻断 SHP1 活性能够增强树突细胞启动 T 细胞的功能。

进一步研究显示,抑制 SHP1 基因,能够模拟维生素E治疗的结果,增加抗原呈递、刺激 T 细胞抗肿瘤免疫反应。同样,抑制 SHP1 可增强树突细胞释放的细胞外囊泡中的抗原呈递,这是树突状细胞和 T 细胞之间的一种重要通讯模式。
靶向 SHP1 可能是一种新的治疗策略
由于维生素E似乎可以改善树突状细胞的抗原呈递,研究团队进一步研究了维生素E是否可以增强已知释放肿瘤抗原和招募树突状细胞浸润的疗法的反应。
实验结果表明,维生素E治疗可以增强癌症疫苗和免疫原性化疗联合检查点抑制剂的效果,包括对免疫治疗耐药的胰腺癌的治疗。
该论文的第一者袁祥良博士表示表示,SHP1 是有效激活树突状细胞以开发有效免疫疗法的有吸引力的靶点。这项研究对维生素E和 SHP1 之间的相互作用提供了重要见解,这将指导我们开发更具体的 SHP1 抑制剂,通过抑制 SHP1 重新激活树突状细胞的抗原呈递可能是增强抗肿瘤免疫的有效策略。
据悉,研究团队目前正在与 MD安德森癌症中心的临床医生合作,以评估维生素E与免疫检查点抑制剂及其他免疫疗法联合的效果。此外,研究团队还在探索开发 SHP1 抑制剂,以及沉默 SHP1 的树突状细胞和树突状细胞来源的细胞外囊泡作为未来新的治疗选择的机会。
原始出处:
Xiangliang Yuan, et al. Vitamin E Enhances Cancer Immunotherapy by Reinvigorating Dendritic Cells via Targeting Checkpoint SHP1. Cancer Discov candisc.0900.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#治疗效果#
40
#患者生存#
41
#Dis#
21
#cover#
38
好文章,谢谢分享。
54
#生存率#
33
#癌症患者#
48
#维生素E#
39
#ISC#
37