Clin Cancer Res:紫杉醇加用Napabucasin治疗晚期胃/胃食管交界腺癌的疗效
2022-08-03 MedSci原创 MedSci原创
紫杉醇加用Napabucasin并不能改善预处理的晚期胃腺癌或GEJ腺癌患者的生存预后
2020年,全球约有110万人确诊胃癌,76.9万人死于胃癌。目前,手术仍是胃癌的唯一潜在治愈性治疗措施。但是,约60%的患者确诊时已是局部晚期或已发生转移。几乎所有晚期胃癌患者经一线治疗后都会发生进展,或表现为原发难治性疾病。
BRIGHTER研究旨在比较紫杉醇加用或不加用Napabucasin(也称为BB608或BBI-608,一种靶向STAT3蛋白的新型靶向药)作为二线治疗晚期胃或胃食管交界(GEJ)腺癌的疗效。
该研究是一项双盲的3期临床试验,受试患者被1:1随机分至Napabucasin(480 mg*2/天)+紫杉醇(80 mg/m2,静脉,3-4周一次)组或安慰剂+紫杉醇组。主要终点是总生存期(OS)。次要终点包括无进展生存期(PFS)、客观缓解率(ORR)、疾病控制率(DCR)和安全性。
总体上,共有714位患者被随机分至Napabucasin组(n=357)和安慰剂组(n=357)。72.1%的男性,74.6%的是胃腺癌,46.2%的已发生腹膜转移。中期分析发生了380例死亡后揭盲。发生了565例死亡后进行了最终疗效分析。
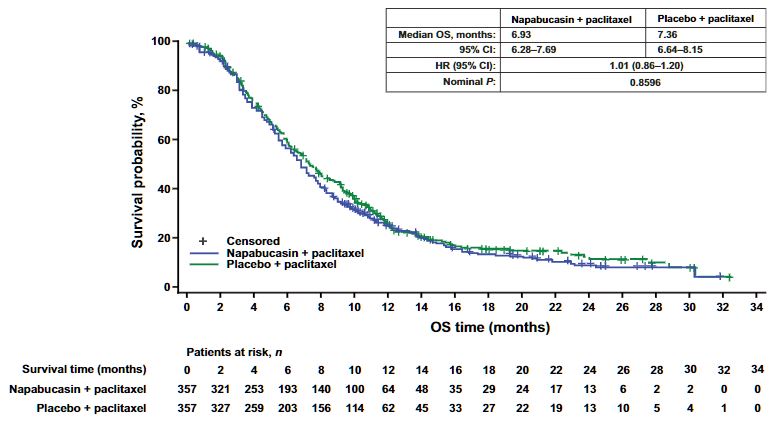
两组的OS率
中位随访了6.8个月。Napabucasin组和安慰剂组的OS(6.93 vs 7.36个月)、PFS(3.55 vs 3.68个月)、ORR(16% vs 18%)和DCR(55% vs 58%)均无显著差异。
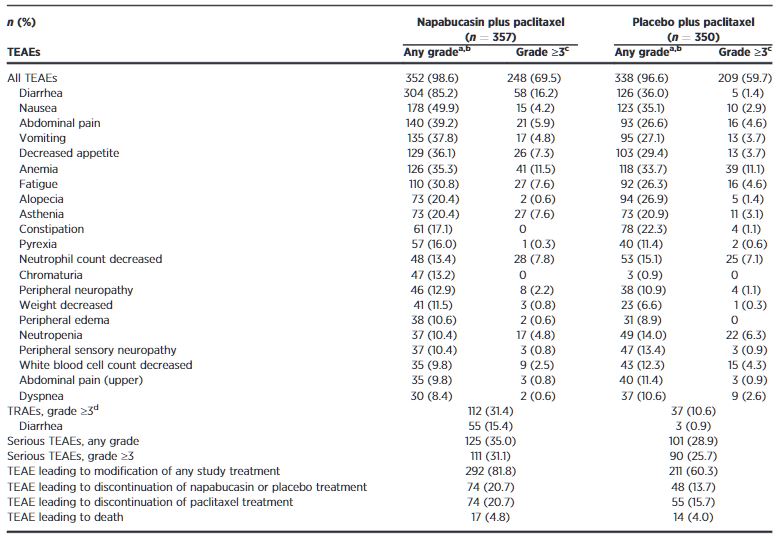
两组的不良反应发生情况
Napabucasin组和安慰剂组3级及以上不良反应的发生率分别是69.5%和59.7%,3级及以上腹泻的发生率分别是16.2%和1.4%。
综上,紫杉醇加用Napabucasin并不能改善预处理的晚期胃腺癌或GEJ腺癌患者的生存预后。Napabucasin的安全性与既往报道的一致。
原始出处:
Manish A. Shah, Kohei Shitara, Florian Lordick, et al; Randomized, Double-Blind, Placebo-Controlled Phase III Study of Paclitaxel ± Napabucasin in Pretreated Advanced Gastric or Gastroesophageal Junction Adenocarcinoma. Clin Cancer Res 2022; https://doi.org/10.1158/1078-0432.CCR-21-4021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#胃食管#
50
#APA#
43
#食管#
31
#Cas#
51