Nat Commun:新分子机制可调节免疫系统的巨噬细胞
2020-04-07 Lauren 转化医学网
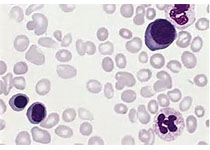
导言:巨噬细胞是一种位于组织内的白血球,它在脊椎动物体内参加先天免疫和后天免疫。巨噬细胞来源于单核细胞,属于免疫细胞。属于不繁殖细胞群。它的主要功能是先固定细胞或游离细胞的形式,然后对细胞残片及病原体
导言:巨噬细胞是一种位于组织内的白血球,它在脊椎动物体内参加先天免疫和后天免疫。巨噬细胞来源于单核细胞,属于免疫细胞。属于不繁殖细胞群。它的主要功能是先固定细胞或游离细胞的形式,然后对细胞残片及病原体进行吞噬以及消化,并激活淋巴球或其他免疫细胞,让它对病原体做出反应。巨噬细胞能够吞没、破坏受损组织,帮助启动康复过程。
国家心血管研究中心(CNIC)团队和纽约西奈山医院的研究者们一起研究,发现了一项通过核受体介导的新的分子机制,核受体能够决定巨噬细胞的特性和扩散。巨噬细胞是人体中充当免疫哨兵的一种细胞类型。这项新的发现机制尤其会影响浆膜腔内的巨噬细胞的。浆膜腔是包围和保护很多器官的膜包围的腔。这一发现在4月3日发表在《自然通讯》杂志上,对影响浆膜腔和浆膜腔所包含的器官的疾病的治疗有非常重要的指导作用。这些疾病包含多种癌症和心肌梗死。
巨噬细胞是免疫系统细胞,主要功能就是在身体内充当哨兵,抵御病原体的入侵。吞噬细胞也能维持体内平衡,通过清除组织修复过程中所产生的组织废物和碎片,从而保持机体系统的平衡和稳定运转。研究协调员兼CNIC核受体信号组组长梅赛德斯·里克特(Mercedes Ricote)博士解释说。近年来,许多研究小组的工作改变了人们对巨噬细胞造血起源和调节的认识。这些研究揭示了组织巨噬细胞之间的巨大异质性,这取决于它们的胚胎或造血来源,以及调节它们的特性和在成年生活中维持的微环境信号。”
有三层浆膜:覆盖腹腔的腹膜;胸膜,包围着肺;还有覆盖心脏的心包。“巨噬细胞驻留在这些空腔中的主要功能之一是通过清除死亡细胞来维持体内平衡,”里克特博士解释说。此外,最近的研究表明,这些巨噬细胞可以浸润邻近的受损器官,“产生一种有效的快速修复反应,不依赖于巨噬细胞前体通过血液供应的补充。”
《自然通讯》的研究是由国立心血管研究中心的里克特博士和在西奈山医院的米里亚姆·梅拉德(Mirian Merad)博士领导,联合共同第一作者Maria Casanova博士(西奈山)和MaPiedad Menende博士(CNIC)所做的研究。研究表明,出生后腹膜巨噬细胞的扩张及其在成年期的维持都受黄素X受体(RXR)控制,黄素X受体是核受体家族的成员。
“RXR存在于细胞内部,”MaPiedad Menende博士解释说,“它检测到存在的脂质和衍生品的维生素a。这些配体激活RXR,触发了特定基因的表达,这些基因能够控制生长,产生免疫,维持体内平衡和保持新陈代谢。”
研究小组发现,RXR需要通过控制新生小鼠浆液腔中巨噬细胞的增殖来建立巨噬细胞群。研究还表明,RXR对成年巨噬细胞的存活也很重要。正如梅内德斯博士解释的那样,“浆液腔巨噬细胞中RXR的缺失会导致大量的有毒脂质积聚,并通过一种叫做凋亡的过程杀死细胞。”
里克特博士解释说,利用小鼠卵巢癌模型,研究表明腹膜巨噬细胞可以浸润卵巢肿瘤,并充当支持肿瘤生长的“肿瘤相关巨噬细胞”。
研究结果表明,RXR功能的丧失导致腹膜腔内巨噬细胞数量的减少,导致这些巨噬细胞对卵巢肿瘤生长的贡献减少,延缓了疾病的进展。里克特博士强调说:“因此,浆液腔巨噬细胞可能成为治疗浆液腔器官受影响的癌症的靶点。”
研究人员对用药物调节RXR的可能性特别感兴趣,包括一些目前用于治疗皮肤淋巴瘤的药物。“我们的研究可能对治疗浆液腔巨噬细胞导致疾病进展的疾病(如癌症),或修复受损组织(如心肌梗死)具有意义。”
原始出处:
María Casanova-Acebes, María Piedad Menéndez-Gutiérrez, Jesús Porcuna, et.al. RXRs control serous macrophage neonatal expansion and identity and contribute to ovarian cancer progression. Nature Communications 03 April 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#新分子#
35
#COMMUN#
31
#Nat#
37
学习了
88
111111111111111111
83
机制研究离临床仍然有距离,不过与临床结合思考,仍然有帮助的,不能仅仅是纯临床思维,转化思维同样重要
58