J Hypertens:血压变异性随着慢性肾脏病分期增加而变大!
2018-03-01 xing.T MedSci原创
由此可见,在这个大型队列中,随着CKD分期的增加,短期收缩压变异性增加。收缩压变异性的增加可能与肾功能恶化引起的心血管风险急剧升高有关。
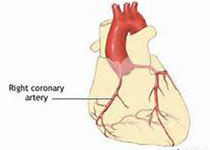
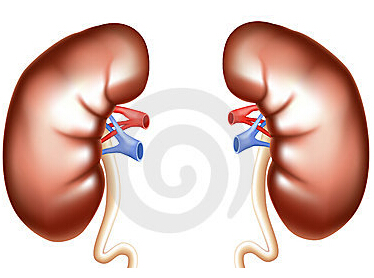
增加的血压变异性可预测高血压患者心血管疾病的发病率和死亡率。近日,高血压领域权威杂志Journal of Hypertension上发表了一篇研究文章,该研究旨在评估根据肾功能分期的短期血压变异性。
研究人员从西班牙的动态血压监测(ABPM)登记中心招募了16546例[10270例(62.1%)无1-5期CKD患者/6276例(38.9%)1-5期CKD患者]受试者。研究人员根据K/DIGO标准定义CKD分期,基于估计的肾小球滤过率,通过CKD-EPI方程和白蛋白/肌酐比值来计算。血压变异性采用标准差(SD)、加权SD(wSD)、变异系数(CV)和平均实际变异性(ARV)来进行评估。
与无CKD的患者相比,较低比例的CKD患者表现为杓状(51.9 vs. 39.6%;P<0.001)。在整个CKD分期中,杓状逐渐减少(从39.1到20.4%,P<0.001)比例又显著增加(从12.3到36.7%,P<0.001)。CKD患者有显着较高的收缩压SD、WSD、CV和ARV和较低的舒张压SD,与无CKD患者相比(P<0.001)。在CKD分期中,研究人员可以观察到从1期到5期,研究人员可以观察到收缩压SD(从13.8±3.7到15.6±5.4mmHg)、wSD(从12±3.2到13.9±5.1mmHg)、CV(从10.4±2.7至11.5±4.1%)和ARV(从9.9±2.3至11.4±3.2mmHg)呈增加趋势;所有的比较P<0.001。而从1期到4期,舒张压SD(P<0.001)、WSD和ARV(P=0.002)稍有降低,而舒张压CV逐渐增加(P<0.001)。在多变量分析中,男性、较大年龄、腹型肥胖、糖尿病、降压药的数量和临床收缩压是CKD患者收缩压24小时ARV的独立因素。
由此可见,在这个大型队列中,随着CKD分期的增加,短期收缩压变异性增加。收缩压变异性的增加可能与肾功能恶化引起的心血管风险急剧升高有关。
原始出处:
Sarafidis, Pantelis A,et al. Blood pressure variability increases with advancing chronic kidney disease stage: a cross-sectional analysis of 16 546 hypertensive patients.Journal of Hypertension. 2018. https://journals.lww.com/jhypertension/Abstract/publishahead/Blood_pressure_variability_increases_with.97520.aspx
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#PE#
35
#TENS#
34
#慢性肾脏#
26
#变异#
27
学习了
65
谢谢分享.学习了
57
学习谢谢分享
80
阅
59
学习了很有用
0
学习了很多先进的医学研究
27