European Radiology:深卷积神经网络在预测HCC患者术前微血管浸润和临床预后方面的价值
2021-12-28 shaosai MedSci原创
肝细胞肝癌(HCC)的根治性切除术是早期HCC患者的第一选择。然而,术后2年的复发率很高,达到50%。
肝细胞肝癌(HCC)的根治性切除术是早期HCC患者的第一选择。然而,术后2年的复发率很高,达到50%。微血管侵犯(MVI)是肿瘤侵袭性、切除后肿瘤复发和生存率较低的一个重要指标。
影像学有助于预测HCC的MVI。深度学习是人工智能(AI)的一个子集,可以自动学习样本图像中的特征表示,可应用于医学的图像识别和判析,其中高性能深度卷积神经网络(DCNN)是新兴的技术之一。然而据我们所知,基于DCNN的MVI的诊断和预后方面的文献有限,需要进一步的研究进行评估。
近日,发表在European Radiology杂志的一项研究本探讨了DCNN在大量HCC手术候选人中使用对比增强CT扫描(CECT)识别MVI以及预测临床预后的性能,为临床术前的准确评估及质量方案的制定提供了影像学参考依据。
本项回顾性研究包括1116名接受术前CECT和根治性肝切除术的HCC患者。根据临床放射学因素、DCNN概率和所有因素,分别在训练队列(n = 892)中构建了放射学(R)、DCNN和组合列线图;每个模型的性能在验证队列(n = 244)中得到确认。计算了预测MVI的准确率和AUC,并记录了手术后的无病生存(DFS)和总生存(OS)。
在训练和验证队列中,MVI阳性患者的比例分别为38.8%(346/892)和35.7%(87/244)。在训练队列中,R、DCNN和组合列线图的AUCs分别为0.809、0.929和0.940,在验证队列中为0.837、0.865和0.897。在训练组(p < 0.001)和验证组(p = 0.009),组合列线图的表现优于R列线图。在R、DCNN和组合列线图预测的有MVI和无MVI的组别中,DFS和OS有显著差异(p < 0.001)。
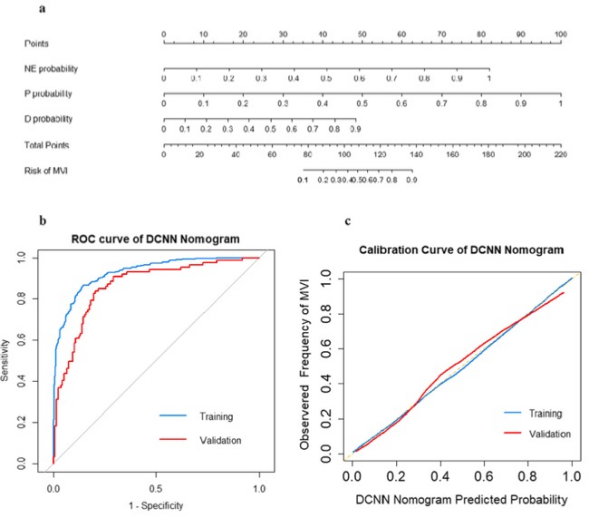
图 a 使用三期相DCNN概率构建的DCNN列线图。 b DCNN列线图在训练和验证队列中预测MVI的ROC分析曲线。DCNN,深度卷积神经网络;MVI,微血管侵袭。
本研究通过结合临床因素和基于术前CECT的放射学特征建立了一个联合列线图,可用于术前预测MVI。同时,该组合列线图还可以预测DFS和OS,为临床个性化治疗方案的制定提供了无创影像学参考依据。
原文出处:
Xinming Li,Zhendong Qi,Haiyan Du,et al.Deep convolutional neural network for preoperative prediction of microvascular invasion and clinical outcomes in patients with HCCs.DOI:10.1007/s00330-021-08198-w
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#PE#
29
#HCC#
54
#微血管#
40
#临床预后#
41
#神经网络#
46