JACIP:Dupilumab治疗减少成人中度至重度特应性皮炎的住院治疗
2022-01-26 医路坦克 MedSci原创
特应性皮炎(AD)是一种慢性炎症性皮肤病,难治性AD可能需要住院治疗,dupilumab治疗与对照组相比,AD相关住院率显着降低,AD相关住院时间缩短。

特应性皮炎(AD)是一种慢性炎症性皮肤病,难治性AD可能需要住院治疗,严重AD发作(恶化)和感染,特别是但不限于皮肤感染。在美国的一项研究中,18.9%的成年人入院时主要诊断为AD或湿疹,并伴有皮肤感染,而没有AD或湿疹的成年人只有4.3%。与无皮肤感染的AD患者相比,AD患者的皮肤感染与住院率和费用显着增加有关。更严重的AD与更高的住院费用有关。此外,约有五分之一的AD相关住院患者(儿童和成人)会在一年内接受第二次住院治疗。中度至重度AD的治疗方案包括各种全身性免疫抑制剂,其中一些可能增加感染风险和需要住院治疗的严重感染。然而,dupilumab是一种完全人类单克隆抗体,可阻断白细胞介素-4和白细胞介素-13的共同受体成分,在成人,青少年和年龄较大的儿童中表现出疗效并且耐受性良好。
我们通过对来自7个安慰剂对照随机对照试验(包括2932名患者)的汇总数据进行事后分析,比较了用dupilumab治疗的中度至重度AD患者与对照组的住院率。
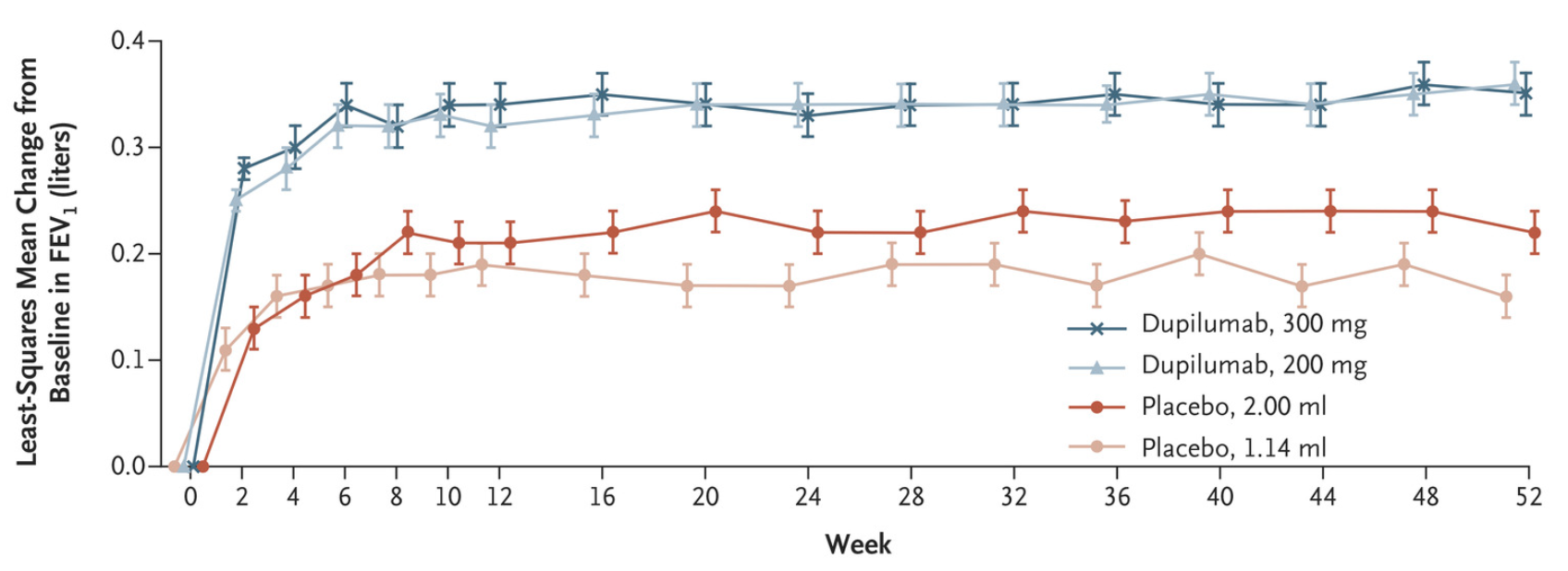
方法:分析7项dupilumab随机,安慰剂对照试验(每2周300 mg[q2w]和/或每周[qw];有或没有局部皮质类固醇)的数据。
结果:dupilumab 300 mg q2w,qw,联合dupilumab(q2w和qw,n=1841)组与对照组(n=1091)患者相比,全因住院率较低(分别为5.8,2.7和3.8事件,而每100例患者为9.0事件-年[PY];所有P<.05[分别为49%,71%和62%的风险降低]);与AD相关的住院治疗(2.0,0.4,1.0事件vs 4.1事件/100 PY;qw和dupilumab合并P<0.05[分别降低风险91%和79%]);以及减少AD相关住院的总体持续时间(10.9,7.3和8.6天vs 38.9天/100 PY)。
在中度至重度AD患者中,dupilumab治疗与对照组相比,AD相关住院率显着降低,AD相关住院时间缩短。
文献来源:Silverberg JI, Rubini NPM, Pires MC,Dupilumab treatment reduces hospitalizations in adults with moderate-to-severe atopic dermatitis.J Allergy Clin Immunol Pract 2022 Jan 12;

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#mAb#
29
#中度至重度#
46
#Dupilumab#
41
#中度至重度特应性皮炎#
32
学习了
45
学习#学习#
44