Biomed Phar:豨莶通栓胶囊减轻慢性脑低灌注大鼠血管性认知功能障碍
2021-11-24 Vivi MedSci原创
豨莶通栓胶囊主要用于急性期和恢复期缺血性中风(脑梗塞)中经络患者,对慢性脑低灌注的保护作用鲜有报道。本研究探讨豨莶通栓胶囊对慢性脑低灌注认知功能障碍的作用及其机制。
研究背景:慢性脑低灌注(CCH)引起的血管性认知障碍的病例逐年增加,但目前尚无临床有效的治疗方法。目前,豨莶通栓胶囊(XXTS)主要用于急性期和恢复期缺血性中风(脑梗塞)中经络患者,但其对CCH的保护作用鲜有报道。
研究目的:探讨豨莶通栓胶囊对CCH认知功能障碍的作用及其机制。
研究方法:52只SD大鼠随机分为假手术组、CCH组和CCH+XXTS组,采用双侧颈总动脉闭塞法(BCCAO)建立SPF级雄性SD大鼠CCH模型。豨莶通栓胶囊于BCCAO术后灌胃42 天。在BCCAO手术后37-42天使用Morris水迷宫测试评估大鼠的认知功能,在术后第43天取血清检测凝血功能(APTT、PT、TT、FIB),脑脊液和血浆检测促炎因子的水平(IL-1α、IL-1β、IL-10、IL-12p70、IL- 17a、IL- 18、CXCL1、GM-CSF、IFN-γ、IL-33、TNF-α、IL-6和MCP-1),免疫荧光染色观察脑白质损伤及神经元情况。
研究结果:三组大鼠血浆PT、APTT、TT、FIB无显著差异,说明长期灌胃豨莶通栓胶囊可能不会影响这些大鼠的凝血功能。大鼠在BCCAO术后出现明显的认知功能障碍,表现为水迷宫测试中现CCH大鼠的游泳轨迹不规则,而CCH+XXTS组大鼠的游泳轨迹有显著改善,豨莶通栓胶囊干预可改善大鼠认知功能障碍。
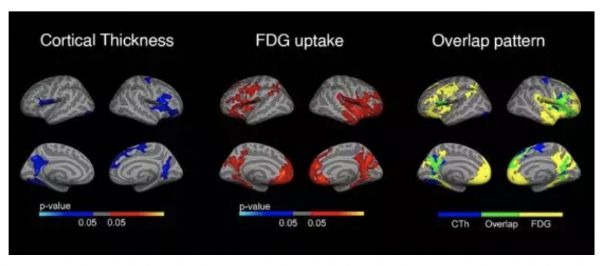
胼胝体中,CCH组MBP荧光强度、细胞计数,NF200细胞计数明显低于假手术组,CCH+XXTS组高于CCH组。纹状体中,与假手术组相比,CCH组MBP、NF200形态疏松甚至断裂,脱髓鞘严重受损。此外,CCH组MBP的荧光强度、细胞计数和NF200的细胞计数均显著下降;CCH+XXTS组MBP和NF200形态趋于完整,与CCH组相比,MBP的荧光强度、细胞计数、NF200的细胞计数均显著增高。
神经元标记MAP2、NeuN的双重免疫荧光染色发现,与假手术组相比,MAP2和NeuN在大脑皮层和海马区的荧光强度显著削弱,细胞的排列松散无序,神经元数量显著减少;而XXTS治疗能显著改善这种趋势,提示豨莶通栓胶囊干预可缓解脑白质损伤及神经元丢失。
此外,CCH组脑脊液中TNF-α、IL-33表达明显高于假手术组,豨莶通栓胶囊干预后,IL-6、TNF-α、IL-33、MCP-1的表达显著低于CCH组。CCH+XXTS组血浆中IL-6的表达明显低于CCH组,TNF-α的表达显著低于假手术组和CCH组,其他血浆炎症因子在三组间无显著差异。
研究结论:豨莶通栓胶囊通过预防脑白质损伤,减少神经元损失,抑制促炎因子表达,改善CCH大鼠血管认知功能障碍。该研究为临床应用豨莶通栓胶囊治疗慢性脑缺血提供了新的参考。
文献来源:
Yan Feng., Tian Yue., Huang Yuyou., et al.(2021). Xi-Xian-Tong-Shuan capsule alleviates vascular cognitive impairment in chronic cerebral hypoperfusion rats by promoting white matter repair, reducing neuronal loss, and inhibiting the expression of pro-inflammatory factors. Biomed Pharmacother, 145(undefined), 112453. doi:10.1016/j.biopha.2021.112453.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Bio#
32
#血管性#
44
#功能障碍#
37
#Med#
33