Cardiovasc Diabetol:空腹甘油三酯水平与2型糖尿病发病率的关系
2022-09-04 从医路漫漫 MedSci原创
需要更好和更早地识别高危个体,特别是考虑到生活方式干预延缓2型糖尿病发病的潜在成功。
背景:2型糖尿病是世界范围内发病率和患病率呈上升趋势的常见病。受影响的患者的发病率和死亡率大幅增加,这不仅会导致个人痛苦,而且还会带来巨大的医疗费用。需要更好和更早地识别高危个体,特别是考虑到生活方式干预延缓2型糖尿病发病的潜在成功。在心血管领域,甘油三酯水平作为血脂异常的生物标志物目前受到越来越多的关注,高甘油三酯血症(高于150 mg/dL)逐渐与不良后果相关。对于偶发的2型糖尿病,甘油三酯主要被认为是高甘油三酯血症作为代谢综合征的组成部分。在这类研究中,甘油三酯正常的参与者通常被用作参照组。循环中的甘油三酯在正常范围内,在没有代谢综合征的情况下,是否也会增加患新发2型糖尿病的风险,目前尚不清楚。
目的:本研究在一个大的普通人群队列的健康参与者中调查了血浆甘油三酯在正常范围内的变化是否与2型糖尿病的发生有关。
方法:肾脏和血管终末期疾病预防研究(PREVEND)是一项来自荷兰北部的前瞻性纵向队列研究[7]。PREVEND得到格罗宁根大学医学中心医学伦理委员会的批准(MEC96/01/022),并根据《赫尔辛基宣言》进行。所有参与者都提供了书面知情同意。年龄在28岁到75岁之间的个人被邀请参加。孕妇和使用胰岛素的受试者被排除在外,剩下8592名参与者进行初步筛查(1997-1998)。5766名参与者有关于2型糖尿病随访和甘油三酯浓度的完整数据,其中总共5665名受试者在基线时没有糖尿病。我们排除了基线时有糖尿病(美国糖尿病协会的定义)或代谢综合征(NHLBI/美国心脏协会的定义)的受试者,空腹甘油三酯>150 mg/dL的受试者(剩余2163人)。确定甘油三酯水平正常的健康个体的2型糖尿病发病情况。
结果:2型糖尿病患病率为3.8%。在线性回归分析中,基线胰岛素、HOMA-IR、总胆固醇、高密度脂蛋白胆固醇、表皮生长因子受体、收缩压(均P<0.001)、血糖、年龄和肌酐(均P<0.01)与甘油三酯在正常范围内独立相关,与甘油三酯升高的预期相当。在Kaplan-Meier分析中,按性别分层的正常甘油三酯与初发2型糖尿病有前瞻性关联(p<0.001)。COX回归证实了独立于HOMA-IR的显著前瞻性关联[HR(95%CI),1.39(1.12,1.74),p=0.002]和其他几个公认的危险因素。
表1向后消除的多元线性回归
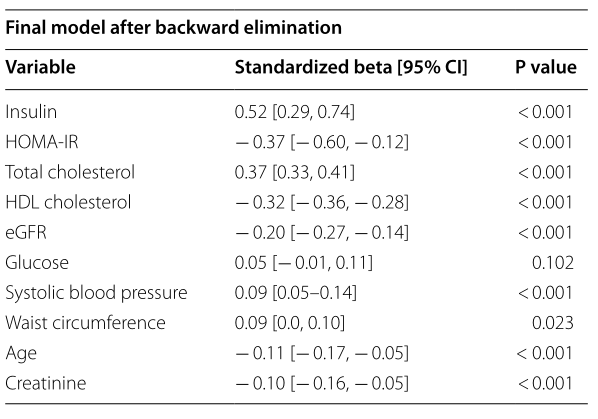
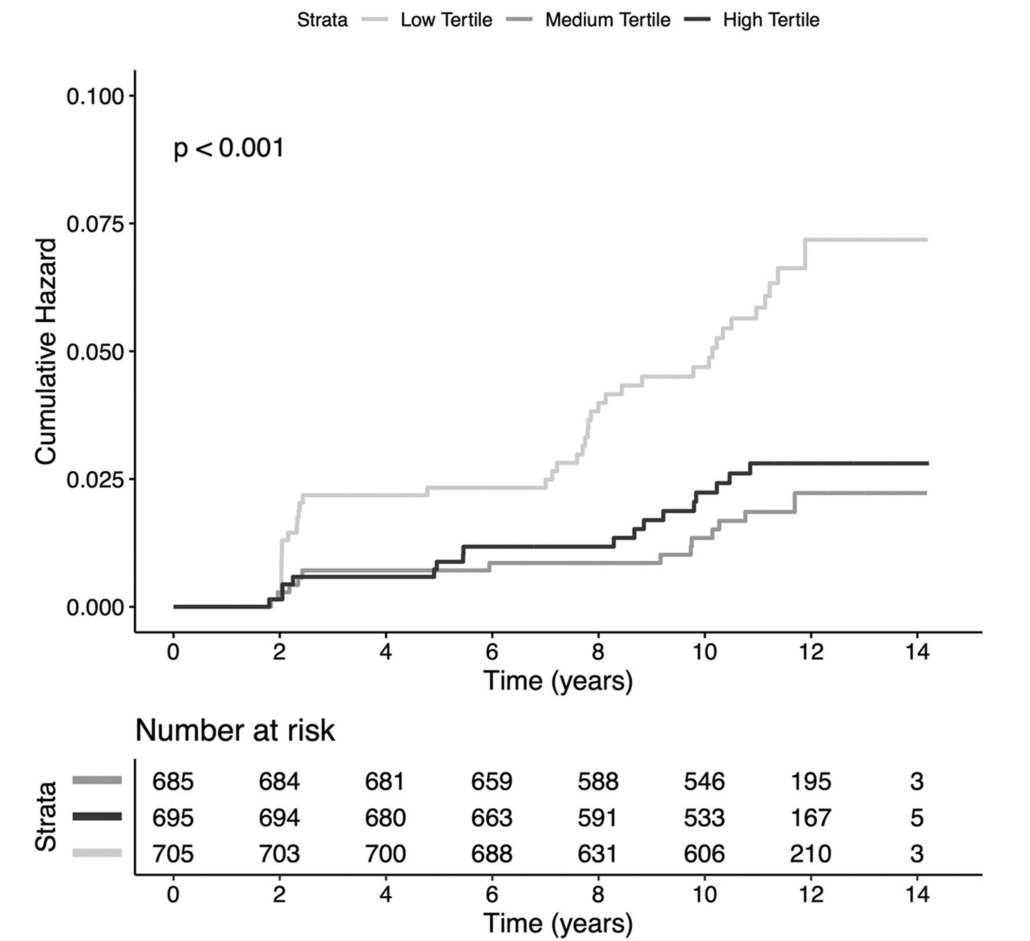
图1 Kaplan-Meier分析根据甘油三酯的三分位数描绘了二型糖尿病(对数秩检验,p值< 0.001)
表2普通人群中正常甘油三酯与二型糖尿病事件的关系
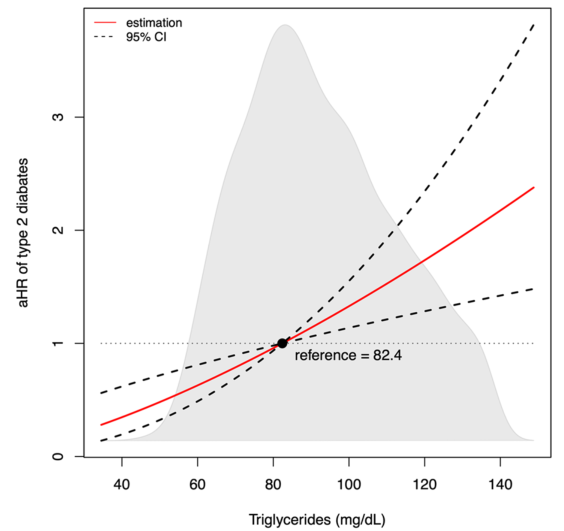
图2根据甘油三酯水平二型糖尿病发展的相对风险。相对风险通过Cox回归分析获得,使用log2转化的甘油三酯,调整年龄和性别。参考值是该队列中血浆甘油三酯的中位数(82.4毫克分升)
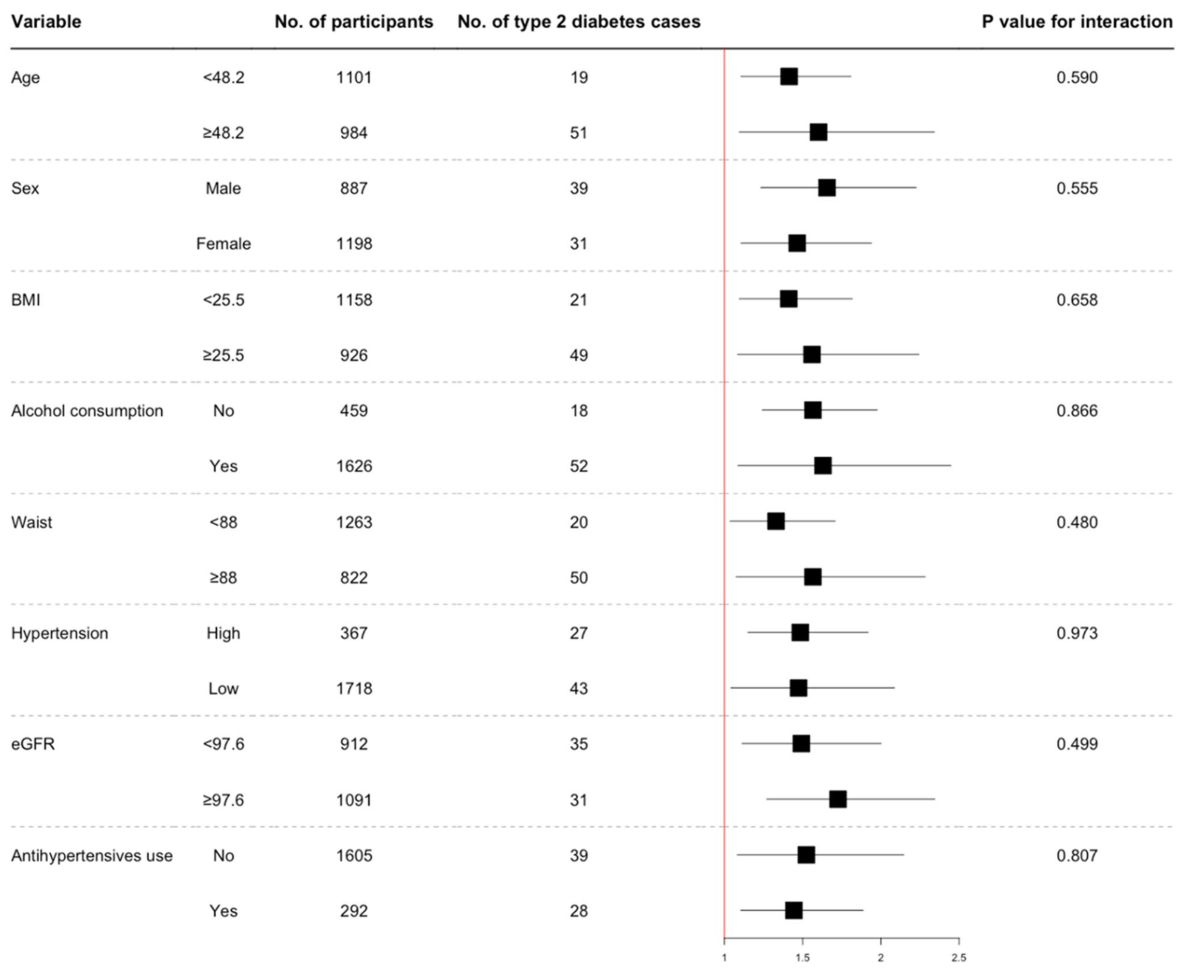
图3几种参与者水平特征的正常血浆甘油三酯值每增加10 mg/dL,二型糖尿病事件的风险比。使用Cox回归分析获得基线甘油三酯浓度与二型糖尿病事件相关的HR (95% CI)。年龄以年为单位,身体质量指数,体重指数(kg/m2);腰围以厘米为单位;eGFR,估计肾小球滤过率(毫升/分钟/1.73平方米)。高血压被定义为收缩压> 140 mmHg
结论:即使在没有代谢综合征的健康受试者中,甘油三酯水平在正常范围内升高也会导致2型糖尿病发病率的持续增加。这些数据表明,几乎每个人都可能从降低甘油三酯中受益,进一步鼓励在普通人群中实施生活方式改变。
原文出处: Szili-Torok T, Bakker SJL, Tietge UJF,Normal fasting triglyceride levels and incident type 2 diabetes in the general population.Cardiovasc Diabetol 2022 Jun 18;21(1)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#BET#
47
#ASC#
25
#DIA#
37
#发病率#
28