胃镜
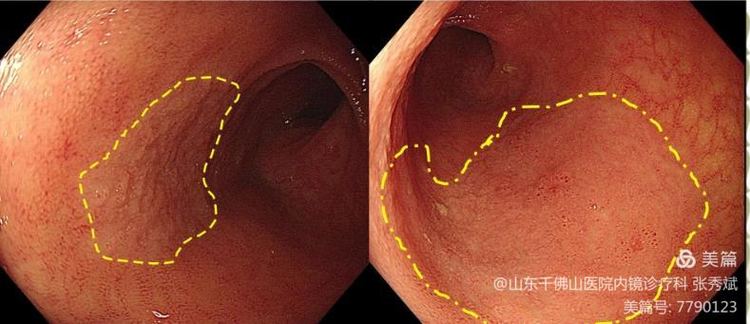
胃镜是食管、胃、十二指肠疾病的最常用检查方法。在胃镜的直视下,可对各种出血病变进行止血治疗;取出胃内异物;对较小的或有蒂的息肉等良性肿瘤可采用圈套、电凝等将其完整切除;对较大的良性肿瘤及早期癌,可根据情况行内镜下黏膜切除或剥离术。胃镜检查结束、患者苏醒后,通常没有不适感。
适应证
(1)有消化道症状,考虑食道、胃、十二指肠溃疡、炎症、肿瘤;
(2)消化道出血,病因及出血部位不明;
(3)其他影像学检查发现上消化道病变,需要明确性质;
(4)上消化道肿瘤高危人群、或癌前病变及癌前疾病普查;
(5)评估溃疡和幽门螺杆菌治疗的效果。
禁忌证
相对禁忌证:
(1)心肺功能不全;
(2)消化道出血,血压波动较大或不稳定;
(3)严重高血压患者,血压偏高;
(4)严重出血倾向,血红蛋白低于50 g/L或PT延长超过1.5秒以上;
(5)高度脊柱畸形;
(6)消化道巨大憩室。
绝对禁忌证:
(1)严重心肺疾患,无法耐受内镜检查;
(2)怀疑有休克或消化道穿孔等危重患者;
(3)患有精神疾病,不能配合内镜检查者;
(4)消化道急性炎症,尤其是腐蚀性炎症患者;
(5)明显的胸腹主动脉瘤;
(6)脑卒中患者。
肠镜
结肠镜主要用于观察从肛门到回盲瓣的所有结直肠的病变。
适应证
(1)腹块,尤其是左下或右下腹块;
(2)慢性腹泻或大便习惯改变者;
(3)不明原因的进行性消瘦伴乏力;
(4)便血或黑便,已排除上消化道的病变;
(5)不明原因的贫血;
(6)锁骨上淋巴结转移性腺癌寻找原发灶;
(7)血清CEA的升高;
(8)钡灌肠或乙状结肠镜发现或疑有病变者;
(9)大肠癌术前的全结肠检查或术后的随访检;
(10)有腺瘤史患者的随访检查;
(11)有大肠癌或腺瘤家族史的直系亲属。
禁忌证
(1)腹腔大动脉瘤;
(2)有腹膜炎或肠穿孔症状者;
(3)严重的心、脑、血管病变者;
(4)活动性出血性降结肠病变;
(5)急性放射性结直肠炎;
(6)晚期癌肿伴盆腔转移或明显腹水者;
(7)腹部或盆腔手术后有严重和广泛肠粘连者。
胶囊内镜
曾几何时,小肠还是内镜检查无法涉足的“禁区”,很多小肠疾病只能依靠剖腹探查或术中内镜等创伤巨大的方法得以诊治。1981年,以色列国防部工程师艾登(Iddan)基于导弹遥控摄像装置的专业背景,萌生研制无线内镜的设想。在1994年的世界胃肠病大会上,Iddan结识了怀有相似创意的英国医生斯温(Swain)。两人迅速成立技术团队,1999年推出胶囊内镜原型,2001年投入临床使用。
这一产品在全世界引起了巨大反响,成为小肠疾病的一线诊断工具。此后,食管胶囊内镜、结肠胶囊内镜也相继问世。胶囊内镜技术开启了消化内镜的无线时代,孕育着极大的发展潜力。
除胶囊内镜外,小肠镜也是小肠疾病诊疗的新发明。2002年,日本学者山本博德与富士写真光机株式会社共同研制出双气囊电子小肠镜。双气囊电子小肠镜在内镜构造和进镜方式上都进行了改良,其不仅能够观察全部小肠,还能在检查过程中进行活检、止血、息肉切除、注射等治疗。
此后,单气囊小肠镜、螺旋式小肠镜也相继问世。小肠镜与胶囊内镜的应用,将小肠疾病的诊治提升到一个新高度。
适应证
(1)不明原因的消化道出血,经上下消化道内镜检查无阳性发现者;
(2)其他检查提示的小肠影像学异常;
(3)各种炎症性肠病,但不含肠梗阻者及肠狭窄者;
(4)无法解释的腹痛、腹泻;
(5)小肠肿瘤(良性、恶性及类癌等);
(6)不明原因的缺铁性贫血。
禁忌证
(1)经检查证实有消化道畸形、胃肠道硬阻、消化道穿孔、狭窄或瘘管者;
(2)体内植入心脏起搏器或其他电子仪器者;
(3)有严重吞咽因难者;
(4)各种急性肠炎、严重的缺血性疾病及放射性结肠炎,如细菌性病疾活动期、溃疡性结肠炎急性期,尤其暴发型者;
(5)对高分子材料过敏者;
(6)18 岁以下、70 岁以上患者以及精神病患者。
推进式小肠镜
与胶囊内镜不同的是,推进式小肠镜因具有吸引及注气的功能,对病变的观察更清晰,发现病变后可以取活检及内镜下治疗;但推进式小肠镜难以观察整个小肠,小肠病变的阳性检出率低于胶囊内镜;且由于检查耗时长,患者较痛苦。因此,多在胶囊内镜初筛发现小肠病变后,需要活检或内镜治疗时才采用推进式小肠镜。
适应证
(1)原因不明的腹痛,经X线钡餐检查无阳性发现或疑有小肠病变者;
(2)原因不明的消化道出血,疑小肠病变者;
(3)疑小肠良、恶性肿瘤者;
(4)小肠吸收不良综合征;
(5)疑小肠淋巴管扩张症。
禁忌证
(1)有胃镜检查禁忌证者;
(2)急性肠梗阻、急性腹膜炎、急性胰腺炎、急性胆道感染等;
(3)腹腔广泛粘连;
(4)严重的心、肝、肾功能不全。
经内镜逆行胰胆管造影
经内镜逆行胰胆管术(ERCP)是在十二指肠镜直视下,经十二指肠乳头向胆总管或胰管内插入造影导管,逆行注入造影剂后,在X线下显示胆系和胰管形态的诊断方法。除诊断外,目前ERCP技术已更多地用于治疗胆胰管疾病,治疗性ERCP包括内镜下乳头肌切开、胆总管取石、狭窄扩张、置入支架、鼻胆管引流术等,其微创、有效及可重复的优势减少了对传统外科手术的需求。
适应证
(1) 胆道梗阻引起的黄疸;
(2) 临床、实验室或影像学检查支持胰腺或胆道疾患(如结石、肿瘤、硬化性胆管炎等);
(3) 胰腺疾病:胰腺肿瘤、慢性胰腺炎、胰腺囊肿等;
(4) 原因不明的胰腺炎;
(5) Oddi括约肌测压;
(6) 胰管或胆管的组织活检。
禁忌证
(1)严重的心肺或肾功能不全者;
(2)急性胰腺炎或慢性胰腺炎急性发作(胆源性除外);
(3)对碘造影剂过敏。
需要强调的是由于CT、超声内镜和核磁共振下胰胆管成像技术(MRCP)的进步,单纯诊断性的ERCP目前很少应用,除非临床上高度怀疑某种疾病并且确实需要 ERCP协助诊断时才考虑应用。
超声内镜EUS
1980年,美国马格诺(Magno)和格林(Green)最先使用内镜与超声结合的电子线型超声胃镜进行实验,并获得成功。随着超声探头的微型化,超声内镜的临床应用变成现实。30年的迅速发展已使之成为一种成熟的内镜诊断技术,使内镜医生的视野超越肉眼限制、拓展到表层组织以下。
目前,超声胃镜、超声肠镜及腹腔镜下超声系统已成功用于临床,尤其是超声内镜引导的细针抽吸术(FNA)等技术可以获取细胞学或组织学标本,对肿瘤TNM分期、黏膜下肿瘤以及胆胰疾病的鉴别诊断有重要意义,极大提高了消化系肿瘤诊断率。
近年,EUS在内镜治疗中的作用日益显现,EUS引导的引流术、腹腔神经节阻滞、放射性125I粒子置入术和顺行胆胰管手术等技术蓬勃发展。
适应证
(1)确定消化道粘膜下肿瘤的起源与性质;
(2)判断消化系肿瘤的侵犯深度及外科手术切除的可能性;
(3)胰胆系统肿瘤;
(4)慢性胰腺炎;
(5)十二指肠壶腹部肿瘤的鉴别诊断;
(6)纵隔病变;
(7)判断食管静脉曲张程度与栓塞治疗的效果。
禁忌证
绝对禁忌证:
(1)严重心肺疾患,无法耐受内镜检查;
(2)上消化道大出血处于休克等危重状态者;
(3)怀疑消化道穿孔患者;
(4)精神病患者或严重智力障碍而不能配合内镜检查者;
(5)腐蚀性食管炎、胃炎的急性期患者;
(6)明显的胸腹主动脉瘤患者;
(7)脑卒中急性期患者。
相对禁忌证:
(1)心肺功能不全;
(2)高血压患者,血压未得到控制;
(3)凝血机制障碍及出血倾向患者;
(4)高度脊柱畸形;
(5)巨大食管憩室、重度食管静脉曲张者。
在过去的历史中,消化内镜技术实现了历史性突破,发展成完整的体系,已达到“无孔不入、无孔造孔而入”的境界,使内镜医师能在无创或微创的条件下进行诊断与治疗。可以说,消化内镜的发明与创新已经将消化疾病的诊断与治疗带入崭新境界,作为一名消化科医生,你最钟爱那一款呢?
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#内镜#
31
技术发展造福人类
38
nb
54
厉害
43
NB
53
学习学习!
35
***
27