动脉血和静脉血常规生化项目是否存在差异?
2019-01-10 严湘红 程歆琦 检验医学网
一、背景&目的 ICU重症患者应用的有创性治疗和检测较多,因此动脉留置导管在ICU病房应用非常广泛,可以为危重病患者提供迅速、直接、准确的血压数据,并可以频繁抽取动脉血标本进行血气分析。
作者:长沙市中心医院检验科 严湘红
北京协和医院检验科 程歆琦
一、背景&目的
ICU重症患者应用的有创性治疗和检测较多,因此动脉留置导管在ICU病房应用非常广泛,可以为危重病患者提供迅速、直接、准确的血压数据,并可以频繁抽取动脉血标本进行血气分析。
同时,重症患者也经常需要做常规生化项目检测,此时往往需要采集静脉血标本。如果动脉留置导管抽取血气标本的同时也能抽取生化项目检测的标本,就可以大大减少静脉抽血次数,减轻患者痛苦和标本溶血的概率,降低重复穿刺诱发感染的风险,这对重症患者来说是十分有益的。因此,在一些大型三甲医院的ICU病房有时会选择使用动脉血标本进行生化项目的检测。
但是,动脉血标本是否能够替代静脉血标本用于常规生化项目的检测,即动脉血和静脉血之间生化项目的检测结果是否有差异呢?因此,我们对动脉血和静脉血标本的生化结果进行了比对研究。
二、结果
动脉血和静脉血标本之间TP、CHE、Glu、TBA、Cr、TG的结果的差异无统计学意义(P>0.05),且上述项目经过回归分析之后,相关系数均在0.98以上。Ca、Cl、K、Na、P、ALB、ALT、AST、LD、Urea、TC和UA的结果的差异有统计学意义(P<0.05)。
同时,我们又根据动脉血和静脉血之间结果的偏差是否超过总允许误差(TE)来判断是否具有临床意义。18个常用生化项目中Ca、Cl、K、ALB、AST、LD和Glu在动静脉血之间的差异临床意义较明显(超过TE的样本比例为10%~90%)。具体见表1、图1。
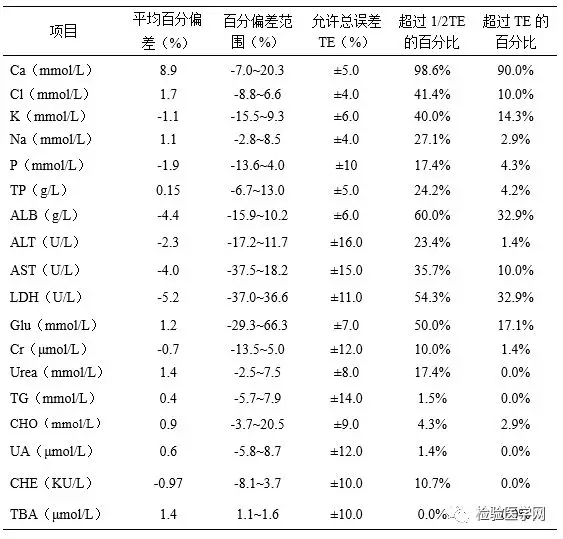
表1:动脉血和静脉血差异具有统计学意义的生化项目的百分偏差分析
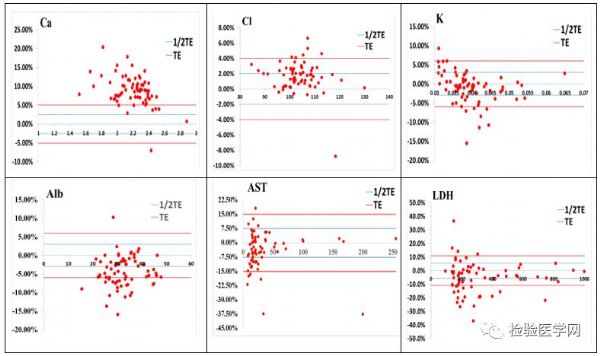
图1:6项生化指标的TE分析图
我们对动静脉血之间差异明显的项目进行了定量比对,结果见图2。

图2:Ca、Cl、K、Alb、AST、LD生化项目的Bland-Altman图。A和V分别示动脉血和静脉血。
三、结论
临床医生如果选择动脉血标本进行上述生化项目的检测,应关注到某些检验项目在动脉血和静脉血之间有比较明显的差异,此时一些建立于静脉血结果之上的参考区间或诊断界值将不再适用,如低钙血症、高钙血症、低钾血症、高钾血症、白蛋白降低等。同时,对于同一患者,如果交替使用动脉血和静脉血进行上述生化项目的监测,以期了解病情变化时,更应关注标本类型对于结果的影响。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#静脉#
42
#动脉血#
34
#静脉血#
39
谢谢分享,学习了
86
学习一下
90