总胆固醇、甘油三酯、LDL-C...血脂报告全面解读!
2022-01-28 综合整理 综合整理
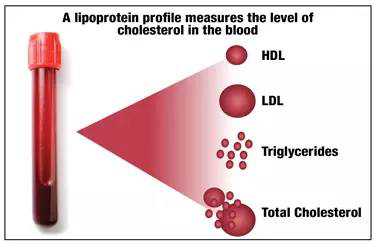
血脂报告单中最重要的四个数值——血脂四项,它的来源以及意义是什么,一起来学学吧。
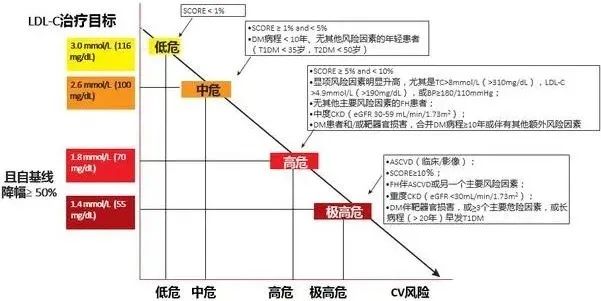
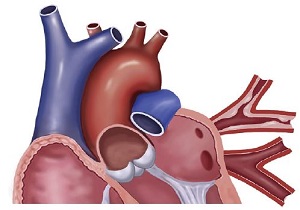
随着经济的发展和人们健康意识的提高,血脂检查已经是大部分体检的必备项目,据统计中国成人血脂异常达到40.4%,控制好血脂水平对于预防心脑血管疾病至关重要。今天这里就向大家介绍一下,血脂报告单中最重要的四个数值——血脂四项,它的来源以及意义是什么,一起来学学吧。 血脂四项包括: 甘油三酯(TG) 总胆固醇(TC) 低密度脂蛋白胆固醇(LDL) 高密度脂蛋白胆固醇(HDL) 什么是血脂 血脂是血浆中脂类物质的总称。脂类物质分为脂肪和类脂,其中脂肪又称有甘油三酯,功能是供应能量和储存能量;类脂包括胆固醇、磷脂、类固醇和糖脂等,功能是维持生物膜的正常结构和功能。 总胆固醇(TC) 血液中所有脂蛋白所含胆固醇的总和,分内源性和外源性。内源性TC由机体自身合成,约50%以上的TC来自机体合成;外源性TC主要来自动物的内脏、蛋黄、奶油及肉等动物性食品。因此,TC受食物的即刻影响较小,是血脂升高的“主犯”。 参考范围:0.0——5.2mmol/L 边缘升高:≥5.2mmol/L且<6.2mmol/L 升高:≥6.2mmol/L 影响TC水平的主要因素有: ①年龄与性别:TC水平常随年龄而上升,但70岁后不再上升甚或有所下降,中青年女性低于男性,女性绝经后TC水平较同年龄男性高。 ②饮食习惯:长期高胆固醇、高饱和脂肪酸摄入可使TC 升高。 ③遗传因素:酶或基因受体基因突变,如家族性遗传性高胆固醇血症,是引起TC显著升高的主要原因。 ④缺乏运动:TC升高常见于动脉粥样硬化、原发性高血脂、糖尿病等。 降低见于恶性贫血、溶血性贫血、甲状腺机能亢进、急性感染,营养不良等。 甘油三酯(TG) TG主要参与人体内能量代谢,产生热能。血中TG含量过高可导致血液黏稠,使脂质在血管壁上沉积,渐渐形成小斑块,即我们平常所说的动脉粥样硬化。TG的主要来源不是肉,而是主食、甜品。通常,对于仅TG高而TC正常的患者,通过调整饮食结构,TG就可能迅速降下来,是血脂升高的“从犯”。 参考范围:0.0——1.7mmol/L 边缘升高:≥1.7mmol/L且<2.3mmol/L 升高:≥2.3mmol/L 同一个体TG水平受饮食和不同时间等因素的影响较大,所以同一个体在多次测定时,TG值可能有较大差异。临床上一般要求空腹测量。TG升高可见于家族遗传性、动脉粥样硬化、冠心病、糖尿病、肾病综合征、胆道梗阻、甲状腺功能减退、急性胰腺炎、糖原累积症、原发性甘油三酯增多症、酗酒;下降一般见于肝性疾病、甲亢等。 低密度脂蛋白(LDL) 参考范围:0——3.4mmol/l 理想水平:<2.6mmol/L 边缘升高:≥3.4mmol/L且<4.1mmol/L 升高:≥4.1mmol/L 影响TC的因素均可同样影响LDL水平。LDL增高是动脉粥样硬化发生、发展的主要、独立危险因素。LDL通过血管内皮进入血管壁内,在内皮下层滞留的LDL被修饰成氧化型LDL(ox-LDL),巨噬细胞吞噬ox-LDL后形成泡沫细胞,后者不断增多、融合,构成动脉粥样硬化斑块的脂质核心。大量研究表明,动脉粥样硬化是一种慢性炎症反应疾病,LDL很可能是这种慢性炎症反应的始动和维持的基本要素。一般情况下,LDL与TC是相平行,但TC水平也受HDL水平影响,故最好用LDL值取代TC,来评估动脉粥样硬化心血管疾病风险。 另外,冠心病患者根据危险分层,降脂目标不同 极高危患者:LDL<1.4mmol/L(55mg/dl)且降幅>50%; 高危患者:LDL<1.8mmol/L(70mg/dl)且降幅>50% 中危患者:LDL<2.6mmol/L(100mg/dl) 低危患者:LDL<3.0mmol/L(115mg/dl) 高密度脂蛋白(HDL) 参考范围:1.16——2.42mmol/L 降低:<1.0mmol/L 由于HDL能将血管壁内胆固醇转运至肝脏进行分解代谢(即胆固醇逆转运),可减少胆固醇在血管壁的沉积,起到抗动脉粥样硬化作用,因此被称为“好”胆固醇。一般认为,HDL与心血管疾病的发病率和病变程度呈负相关。但需要注意的是,高水平的HDL,并非所有情况都一定有益。 HDL的水平明显受遗传因素影响,HDL降低常见于严重营养不良、肝炎、贫血和肝硬化等,而运动和少量饮酒会升高HDL-C。 高血脂的治疗 对于高脂血症患者,饮食治疗和生活方式改善是治疗高脂血症的基础措施。无论是否进行药物治疗,都必须坚持控制饮食和改善生活方式。良好的生活方式包括坚持心脏健康饮食、规律运动、远离烟草和保持理想体重。对于单纯改善生活方式仍无法控制血脂时,应及时给予他汀药物治疗。对于已经发展成为冠心病时,应同时给予抗血小板和抗心肌缺血治疗等。
1. 中国成人血脂异常防治指南修订联合委员会.中国成人血脂异常防治指南(2016 年修订版).中国循环杂志.10(31):937-953.
2.葛均波,徐永健.内科学(第8版).2015;人民卫生出版社.
3.王长谦,顾俊.你知道 血脂四项的秘密吗.家庭医学,2017;1:4-7.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











棒
46
#总胆固醇#
37
清晰
48
学习了
59
实用性强,学习了
57
#LDL#
41
学习学习,很全面
70
学习了
61
学习了
53
学到了
39