DIABETOLOGIA:转录因子STAT6在促进β细胞存活方面起着关键作用
2019-04-04 不详 网络
<span style="font-size:12.0pt;font-family:宋体;mso-ascii-font-family: Calibri;mso-ascii-theme-font:minor-latin;mso-fareast-font-family:宋体;mso-fareast-theme-font: minor-fareast;mso-hansi-font-family:Ca
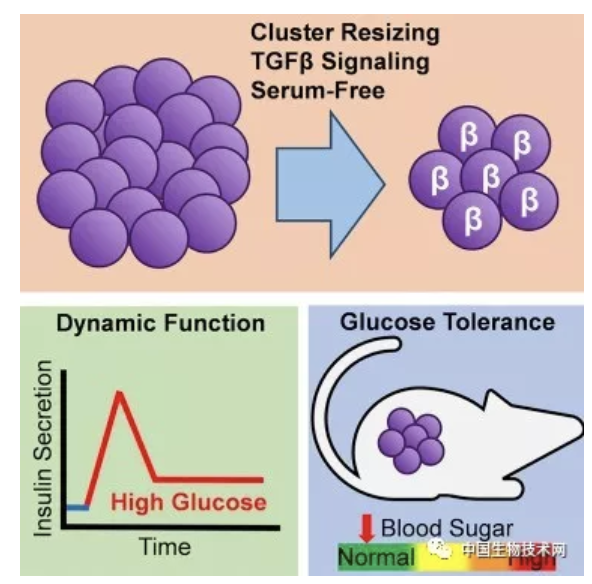
在1型糖尿病中,在炎症性胰岛环境中选择性β细胞丢失发生。这种环境是通过促炎细胞因子的增强分泌和IL-4和IL-13等抗炎分子的丢失而产生的。虽然促炎细胞因子的作用已经在β细胞中得到了很好的研究,但它们的抗炎作用相对较少受到关注。
研究人员克隆β细胞、分离的人胰岛和来自对照个体和1型糖尿病患者的胰腺切片。采用靶向基因芯片和定量RT-PCR检测基因表达。用免疫细胞化学方法检测蛋白在细胞提取物和组织切片中的表达。用干扰RNA选择性地敲除靶蛋白。
结果显示,IL-4和IL-13的细胞保护作用是通过信号传感器的早期激活和β细胞转录因子6 (STAT6)的激活来实现的,从而导致抗凋亡蛋白的上调,包括髓样白血病(mcl1)和B细胞淋巴瘤(BCLXL)。我们也报告的感应信号监管protein-α(SIRPα),并发现敲除SIRPα与β细胞生存能力降低有关。这些抗凋亡蛋白及其伴随的细胞保护作用在sirna介导的下调STAT6后丢失。重要的是,对人类胰腺切片的分析显示,1型糖尿病患者的β细胞中STAT6明显减少,这意味着细胞保护反应的丧失。
研究表明,STAT6的选择性缺失可能在1型糖尿病进展过程中导致β细胞死亡
原始出处:
Kaiyven A. Leslie, Mark A. The transcription factor STAT6 plays a critical role
in promoting beta cell viability and is depleted in islets of individuals with
type 1 diabetes
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#DIA#
25
#转录#
28
#BET#
32
#转录因子#
37
#β细胞#
41