Ther Adv Med Oncol:真实世界数据研究新诊断转移性女性乳腺癌患者中年轻(≦40岁)患者的治疗以及预后
2022-01-25 yd2015 MedSci原创
研究表明,新诊断转移性乳腺癌患者中,年轻患者(≦40岁)的中位OS优于41-69岁患者。不同亚型患者预后差异较大,值得进一步的探讨。
近期,Therapeutic Advances in Medical Oncology杂志上发表了一项来自法国的研究成果,主要是真实世界中探索年轻的(⩽40岁)新诊断转移性乳腺癌女性患者的管理和预后。

研究评估2008年至2016年接受治疗的22,463例40岁女性新诊断MBC的资料(NCT0327531)。主要目标是比较年轻(⩽40岁)和年龄为41-69岁的女性新诊断MBC患者的总生存期(OS)。次要目标是比较一线治疗无进展生存期(PFS1)和描述治疗的模式。
4524例患者符合纳入标准,其中598名(13%)年龄为≦40岁。MBC诊断的中位年龄为36岁(范围= 20 ~ 40岁)。与年龄41-69岁的患者相比,年轻女性更多III级肿瘤(49% vs 35.7%, p <0.0001), ER-肿瘤(30.1% vs 25.1%, p = 0.0090), HER2+肿瘤(34.6% vs 26.4%, p<0.0001)和TNBC肿瘤(17.1% vs 12.7%, p<0.0001)。年轻女性患者原发灶肿瘤手术比例更高繁(41.7% vs 31.6%,p<0.0001)。诊断时肝转移在年轻女性中更为常见(38.1% vs 30.7%,p = 0.0003)。
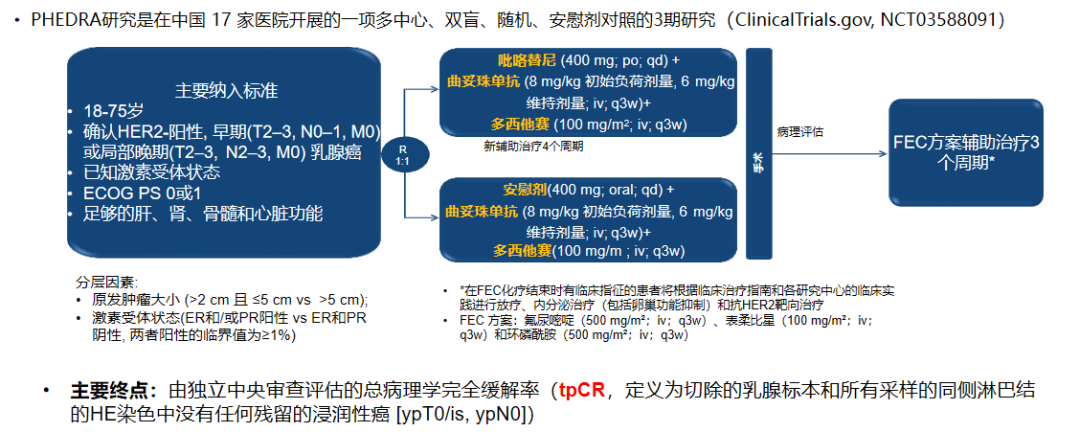
HR+/HER2–患者中,年轻患者大部分(89.6%)一线接受化疗(CT);HR–/HER2–患者中,年轻患者一线治疗包括CT单独治疗(64.7%)或联合贝伐单抗治疗(29.4%);HER2+患者中,年轻患者中196例(94.7%)接受了一线抗HER2治疗,其中80例(40.8%)接受了双阻断抗HER2(曲妥珠单抗+帕妥珠单抗),113例(57.7%)接受了单独曲妥珠单抗。

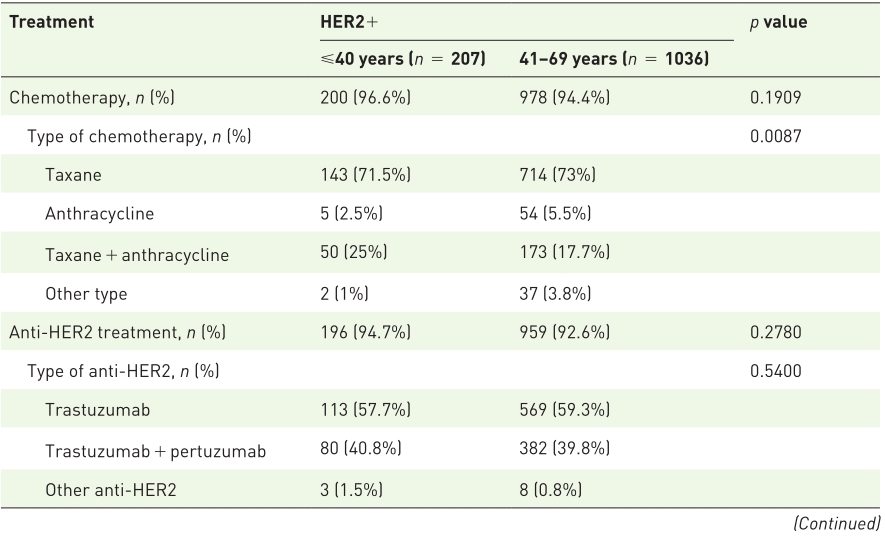
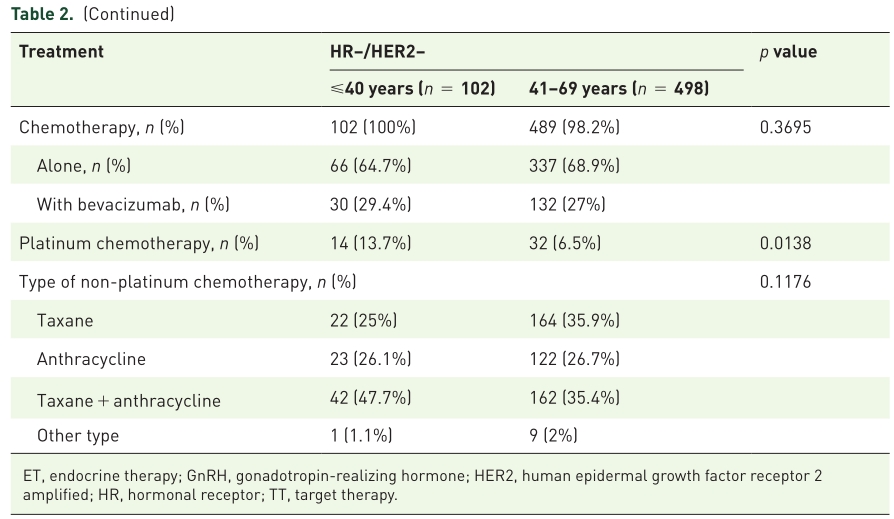
一线治疗
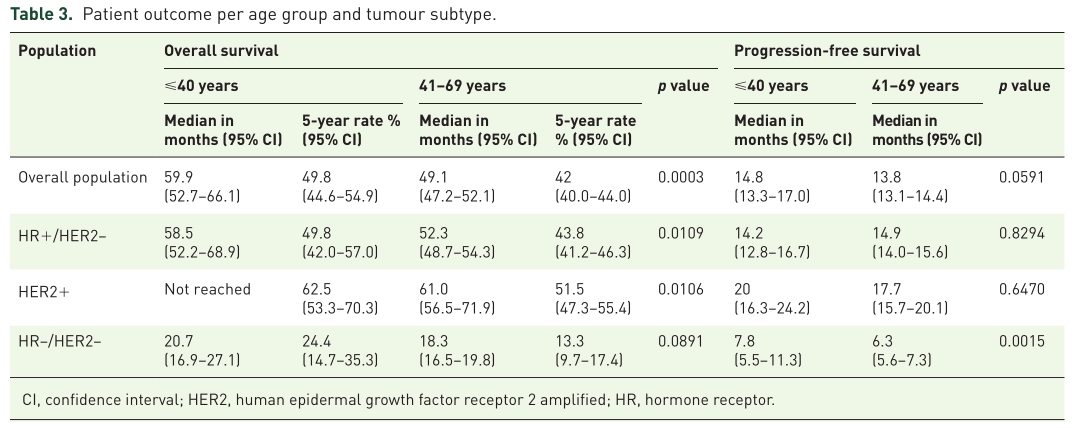
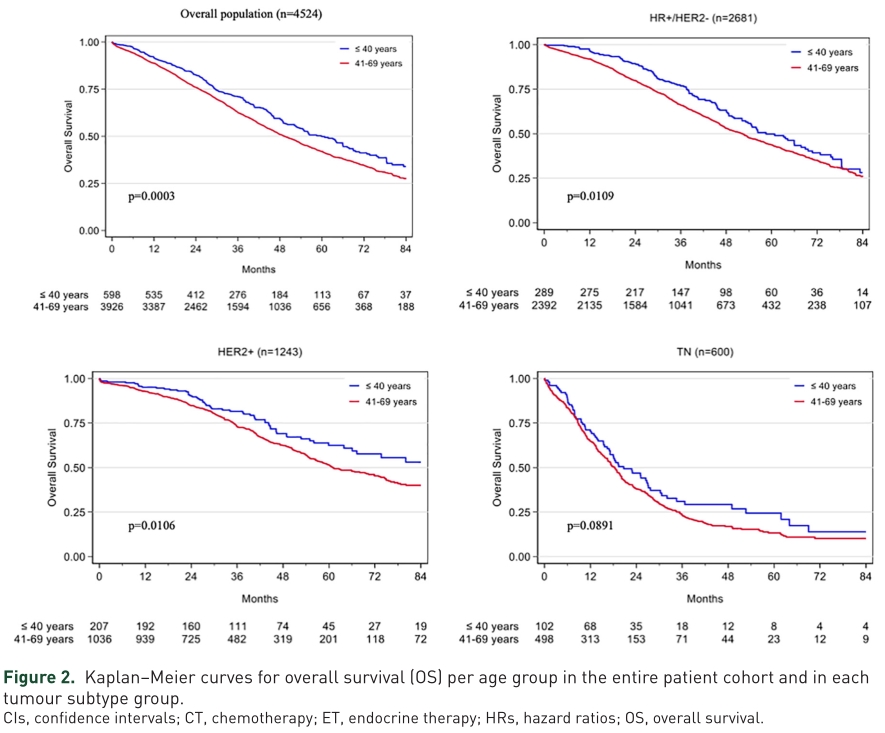
中位随访49.7个月(95% CI = 4851.7),报告了2144例死亡(40岁组为249例,41- 69岁组为1895例)。总体人群、年轻女性和年龄为41-69岁患者的中位OS分别为50.5个月(95% CI = 48.5 -52.9个月)、59.9个月(95% CI = 52.7-66.1个月)和49.1个月(95% CI = 47.2-52.1个月)。与>40岁女性患者相比,年轻女性的5年OS率在数值上更好,HR+/HER2、HER2+和TNBC亚型分别达到50%、63%和24%。
OS和PFS
OS

OS亚组分析
在单变量分析中,年轻、HR+/ HER2和HER2+亚型、低分级(I/II vs . III)、转移部位数量<3和无内脏转移与整体新诊断MBC人群的OS更好相关。在多变量分析中,41-69岁仍是整体人群(HR = 1.28, 95% CI 1.47 = 1.11),HR+ / HER2- (HR = 1.29, 95% CI 1.58 = 1.06)和HER2 +(HR = 1.37, 95% CI = 1.03 - 1.83)人群OS独立预后因素。
≦40岁女性患者中位PFS1为14.8个月(95% CI = 13.3 17.0),而41-69岁女性患者中位PFS1为13.8个月(95% CI = 13.1 14.4),没有无统计学差异( p = 0.0591)。在HR+/HER2-患者中, 年轻患者的一线CT +/–ET治疗的中位PFS1为14.4个月,41-69岁患者的为7.6个月。TNBC患者中, 接受CT + 贝伐珠单抗的中位PFS1分别为4.9和6.4个月。

PFS
在整个人群中,96名患者有BRCA1/2突变,其中44人年龄为≦40岁。年轻的BRCA患者III级肿瘤更常见(63.4%,vs 整体人群为49%)。大多数患者为HR+/HER2-和TNBC肿瘤(分别为52.3%和43.2%),只有2例(4.5%)患者为HER2+肿瘤。与年龄较大的BRCA患者相比,年轻的BRCA女性HR+/HER2-肿瘤较少(52.3% vs 71.2%),更多TNBC肿瘤(43.2% vs 17.3%)。年长的BRCA女性比年轻女性有更多的骨转移(73.1% vs 43.2%,p = 0.0030)。绝大多数年轻和老年BRCA女性接受CT作为一线治疗(97.7% vs 86.5%, p = 0.07)。
综上,研究表明,新诊断转移性乳腺癌患者中,年轻患者(≦40岁)的中位OS优于41-69岁患者。不同亚型患者预后差异较大,值得进一步的探讨。
原始出处:
Amélie Mallet, Amélie Lusque, Christelle Levy,et al. Real-world evidence of the management and prognosis of young women (⩽40 years) with de novo metastatic breast cancer. Ther Adv Med Oncol. 2022, Vol. 14: 1-15.DOI:10.1177/17588359211070362.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Oncol#
41
#新诊断#
26
坚持学习
50
#真实世界#
28
#转移性#
30
#乳腺癌患者#
39
#Med#
22