Nature:在体筛选800多个基因发现阻止癌症转移的新靶点
2017-01-15 生物谷 生物谷
来自英国桑格研究院的一项新研究为遏制肿瘤转移找到了新的药物靶点。相关研究结果发表在国际学术期刊Nature上。这项研究共发现23个参与癌细胞转移调控的基因,研究人员证明靶向其中一个基因——Spns2能够显著抑制肿瘤扩散。肿瘤转移是导致癌症病人死亡的首要原因。高达90%的癌症死亡都因癌症转移而发生,但是目前对癌症转移的调控机制仍了解不足。为了
来自英国桑格研究院的一项新研究为遏制肿瘤转移找到了新的药物靶点。相关研究结果发表在国际学术期刊Nature上。这项研究共发现23个参与癌细胞转移调控的基因,研究人员证明靶向其中一个基因——Spns2能够显著抑制肿瘤扩散。
肿瘤转移是导致癌症病人死亡的首要原因。高达90%的癌症死亡都因癌症转移而发生,但是目前对癌症转移的调控机制仍了解不足。
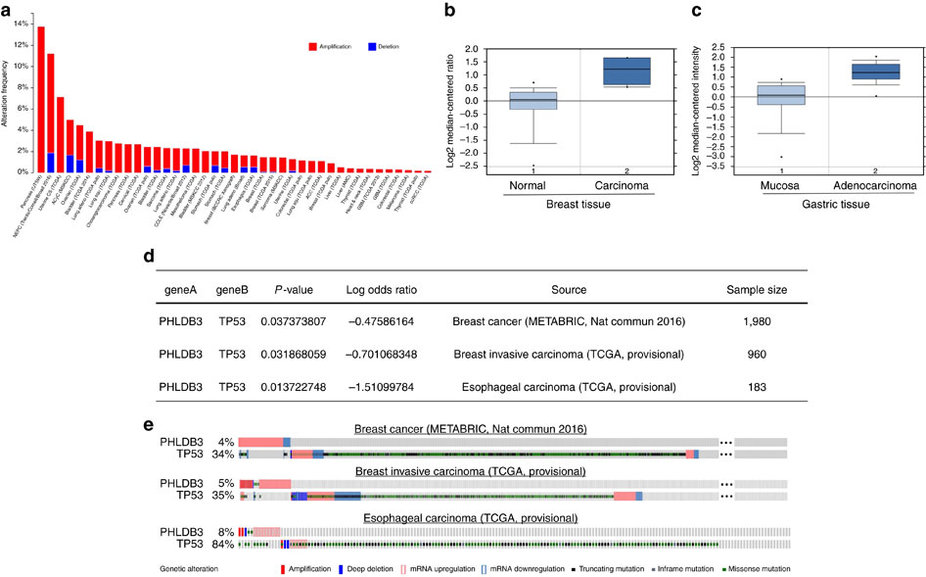
为了找出影响癌细胞转移的基因,研究人员借助敲除了单个基因的多种基因工程小鼠对肿瘤转移过程进行了研究。他们筛选了810个基因在其中发现了23个促进或抑制皮肤肿瘤细胞向肺部扩散的基因。其中的许多基因还会引起免疫系统的变化。
移除Spns2基因会引起最显著的变化,可以大大抑制肿瘤向肺部的扩散。随后研究人员又检测了该基因对其他癌症扩散的作用,包括结肠癌,肺癌和乳腺癌,并发现敲除Spns2也会抑制这几种癌症的转移。
来自桑格研究院的Dr. David Adams这样说道:“Spns2基因的缺失会导致肿瘤转移灶的形成受到显著抑制,因此该基因代表了一个新的药物靶点。我们发现缺失Spns2基因的小鼠其免疫细胞的比例也不同于正常小鼠,似乎该基因的缺失会促进免疫系统清除癌细胞。靶向该基因的药物或许可以帮助抑制或阻止癌细胞向身体其他部位的扩散。”
在该研究之前,有研究发现Spns2基因能够影响免疫系统,但是并未将其与肿瘤扩散联系在一起。该基因编码的蛋白能够对S1P这种脂质进行转运,S1P可以向免疫系统传递信号,在缺少转运蛋白后该信号不能正常运作从而导致机体内不同免疫细胞的比例发生变化。
该研究为抑制甚至阻止癌细胞转移提供了一个新的药物靶点,未来有望借助该方法达到治疗癌症的目的。
原始出处:
Genome-wide in vivo screen identifies novel host regulators of metastatic colonization
Louise van der Weyden, Mark J. Arends, Andrew D. Campbell, Tobias Bald, Hannah Wardle-Jones, Nicola Griggs, Martin Del Castillo Velasco-Herrera, Thomas Tüting, Owen J. Sansom, Natasha A. Karp, Simon Clare, Diane Gleeson, Edward Ryder, Antonella Galli, Elizabeth Tuck, Emma L. Cambridge, Thierry Voet, Iain C. Macaulay, Kim Wong, Sanger Mouse Genetics Project, Sarah Spiegel, Anneliese O. Speak & David J. Adams
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Nat#
32
学习一下很不错
53
相关成果可以选择发表《CancerCellResearch》和《Chronic?DiseasesPreventionReview》期刊征稿,需要发表文章的可以投稿到邮箱editor@cancercellresearch.org
78
科技的进步,人类的发展
49
收藏,学习,进步
62
收藏起来
45
#新靶点#
17
#癌症转移#
18
#筛选#
18